I am now ending my Christmas break and have finally decompressed enough to blog. (Or, I've finally realized that if I don't specifically carve out time to blog, it won't happen and all I will do is hang out with siblings, clean the kitchen, and do errands.) I am now one sixth of the way through internal medicine: two weeks down, ten to go.
Internal medicine (IM or "I med") is the meat and potatoes of the third year: it represents most of Step 2, and it teaches us basics of adult medicine. Our rotation is made up of one week of palliative care, two month-long rotations with an inpatient team of residents, and two weeks of outpatient care with a practicing physician in the community. Because our Christmas break landed in the middle of one of the month-long rotations, I have one fewer inpatient weeks and one additional outpatient week. (Cue the Alleluia chorus, because inpatient is much more intense and demanding than outpatient; this coincidence will give me more time to study and less time with resident team 1, which is keeping me hopping although I'm learning a ton.)
In one week on this residency team, I saw patients with stroke, sickle cell crisis, cellulitis, heart attack, heart failure, pericardial effusion, leukemia, sepsis, coma, and disseminated cancer. One patient died (I was not present).
The resident quizzes us a lot during the day, so studying is a must. We write notes on the three patients we see, and we see them before 8:00am, which means I'm getting up at 5:00, and that also means I'm usually missing Mass. I'm struggling to work until 5:00pm or 6:00pm, study, pray, and relax. IM is challenging me!
Formation is stressing living as Christ and being the Eucharist for others, though, so I am definitely getting a chance to do that. And St. Faustina says that one Eucharist lasts until the next, so I'm at peace as far as Mass goes. Praying the litany of humility (and just being a third year med student) is also helping me have realistic expectations of what I can and can't do, and how much I should or shouldn't know at this time in my life.
In other news, all during the OB/GYN rotation I either avoided or bumbled through explaining why I wouldn't prescribe contraceptives. Today, at coffee with my high school friends, one of them asked me about it and I explained *~beautifully~* why I thought what I did. Yay! I can have that conversation! (One down, a million to go.)
Saturday, December 28, 2013
Wednesday, December 4, 2013
Bizarre, Unsurprising, Pitiable, Absurd: a lecture on Homosexuality
I went to a mandatory lecture about homosexuality. (It wasn't relevant to medicine, although it was supposed to be.) My notes on his lecture have three phases: dutifully recording the bizarre but natural consequences of his ideas, pity for a man who was still clinging to an outdated and dystopian revolution, and shaking my head as he reduced himself to the absurd.
Forty Years I endured this Generation. That's Enough.
Nonsense is Nonsense
Big Surprises: NOT.
- The lecturer admitted freely and happily that the LGBT community was vague. (The T was added in the '90's, another T for T-squared added shortly thereafter, then I for intersex, then Q for questioning and another Q for queer....) No one could agree on what the community was really made up of, or who should be in or out, or whether membership was permanent, or whether people who didn't want to be in were in based on criteria that admitted others who wanted to belong. No surprise to me and to anyone who knows what separation from objective truth can mean. Look at the fallout of the Reformation! Of course legitimizing a falling away from man's natural inclination will result in chaos.
- He discussed the possibility of "polyamorous communities," or "open marriages" (his words). Again: surprise? This is an old reality with a new name. It used to be called cheating, but it's the new normal. I can forsee it happening very soon, since the youth who grew up in the hookup culture (basically a culture of polyamour) will likely live the same habits later in life. The sad thing is, love with many is love with none. When human love isn't exclusive and irrevocable, it's not love.
- Still on the topic of "open marriages," he said that marriage is "not just for individual beauty...but also for children," meaning that consenting adults should reap not only the enjoyment of sex, but the enjoyment of children, too. But in this, he subtly states that children aren't individuals. He next stated that "open marriages" would involve "lots of complexity that kids have to deal with." Again, no surprise: we have been treating children as less than human for nearly half a century: first, the unborn, then, the born. Now, we just speak about it openly.
Forty Years I endured this Generation. That's Enough.
- "The whole notion of labels [is] melting before our eyes...beginning to thaw and melt away." When the lecturer said this, I simultaneously pitied him and felt anger. I pitied him because he's so behind: that battle cry rose almost a century ago and now plays as cheap background music in the minds of everyone under (at least) forty. And I was angry, because this attitude has played out its destruction on my generation. The lecturer said, "my goal is to disrupt society" and "deconstruct statutes." But society is already deconstructed. My generation might say to the lecturer's, "We were raised in divorces or among divorces, breathing relativism and drinking perpetual self-absorption and agnosticism about everything except opinions and sensation. What else would you like to deconstruct?"
- Around this point in the lecture, I wrote in my notes "So Marxist!" And one inch lower on the paper I wrote: "Two minutes later he brought up Marx. [The lecturer] studies [Marx] and says he doesn't believe everything of it." Whatever.
- And then, because this man happened to be a lapsed Catholic, we got a good dose of pancretism, or the choice of religion based on preference of accidents (the lecturer liked Episcopalianism better for several reasons). Yawn.
- The lecturer condemned "the puritan U.S. division of sexual and spiritual," and I was happy to hear it, since puritanism is one of the great errors of our time. But (as with his quotes about thinking deeply) this didn't pan out, since his next idea was excitement about prostitution. At this point in the lecture my notes became frustrated question marks. See above for how my generation is already living prostitution. Again: thanks for the errors.
- "Language is unintelligible," he said, and I can't remember what he said that about. I wanted to snort, "language isn't the only thing that's unintelligible," and not in an ad hominem: nothing is intelligible in relativism. My first question to my peers who want to talk about God is always: do you think we can know anything? (And then, "how?" or "why not?" or "how do you know that?")
Nonsense is Nonsense
- He did such an elegant job of characterizing his position as nonsense that I felt my job was done. He specifically said that this is a first world problem.
- "Other" on forms that list "male" and "female" as genders is offensive. I was so close to laughter.
- In Angels in America, the homosexual patient tells the doctor his diagnosis by the end. He thinks that's a great ending; in a way, so do I. It says outrightly, "we assert our statement over the truth," if you take the physician as the art of medicine personified, a symbol of the objective way the body works.
- He used the word "tragedy" that we did not accept those who did not identify as male or female. Tragedy is a word I use more carefully.
- "Gender and sexuality [are] entirely separated for us," he said, speaking for the LGBT community, I guess. "But that doesn't mean anything." ???
- The lecturer was saying that about 1% of children are intersex, based on some ridiculous data counting boys with hypospadias as intersex. "I personally tend to believe this literature," he said.
- On the last page of my notes, I have written in large handwriting (which happens when I get angry), "WHY are we talking about the ordination of women??" The lecture had devolved and I felt like I was in a Catholic-bashing fest. He exhibited one of his own paintings, which featured a photo of The Ecstasy of St. Theresa, various pornographic photos, and unconsecrated hosts (covering the genitalia of the naked figures). I was upset, but also felt vindicated. I am proud that the Church is ridiculed in the rejection of the truth: she stands with her Spouse.
- The lecturer's last advice: find a community that allows your behavior. But that is backwards. We go into communities to become happy, fulfilled, perfected people, not children.
Monday, November 25, 2013
First Delivery!
 O I just got off 24-hour call, from 7:00am Sunday to 7:00am Monday. It was very eventful: I scrubbed in to four vaginal deliveries and two C-sections. And I delivered my first baby! And guess what his name was? I can't tell you because that would be breaking the law, but it may have been remotely related to one of my favorite people, and that made me really happy. Plus, the couple was really wonderful: the wife was beautiful, and was working really hard and keeping a great attitude the entire time. And the husband was kind and supportive, and when I handed him his child, he started to sniffle (hiding it as best as he could, which was not at all) and hadn't stopped sniffling when I left the room. They were young, and this was their first baby.
O I just got off 24-hour call, from 7:00am Sunday to 7:00am Monday. It was very eventful: I scrubbed in to four vaginal deliveries and two C-sections. And I delivered my first baby! And guess what his name was? I can't tell you because that would be breaking the law, but it may have been remotely related to one of my favorite people, and that made me really happy. Plus, the couple was really wonderful: the wife was beautiful, and was working really hard and keeping a great attitude the entire time. And the husband was kind and supportive, and when I handed him his child, he started to sniffle (hiding it as best as he could, which was not at all) and hadn't stopped sniffling when I left the room. They were young, and this was their first baby.Positives and negatives: I also got shoved away (literally, my hand was boxed out of the field) from an earlier delivery, which was just although a little harsh. It was one of the interns' patients, and the intern had come on her day off between rotations to deliver the patient. I'd seen the patient before, and was just trying to do what our clerkship director told us to do by holding a sterile towel to the perineum. I'm constantly trying to find the "aggressive" that's looked upon as praiseworthy in surgical subspecialties; one one side is true getting in the way or overstepping what we're allowed to do, and on the other side is not getting experiences and looking uninterested or lazy. I guess my upper-level answered that question for me this time: get out of the way, this is the intern's delivery!
I was also in on a delivery where the mother had chorioamnionitis. The mom's body was palpably hot. The baby also had other complications like meconium staining and late decelerations. But her delivery was remarkable for a really supportive family.
The last delivery I was in on last night almost moved me to tears. The mother had been laboring for days in the inactive latent phase. Suddenly, she went from 3 centimeters dilated to completely dilated, and her pushing was extremely effective. She pushed seven times, and her baby was born! She played soft country music from her iPad during her pushing, and she turned the TV off. She had one female friend with her (a friend, not a doula, but serving pretty much the same purpose). What was most remarkable was how strong and clear her emotions were about the delivery: her love for that baby struck me with awe. When the baby was born and I placed it on her chest, her expression and her quiet almost-sobbing words of love made me tear up. And then, when the baby needed a little resuscitation a few minutes later because of some complications (baby is fine now), she was anguished. She controlled her anxiety, but just barely! And she spoke to her baby across the room (where the NICU team had him under a warmer with a respirator) by name, calling out softly and encouraging him to cry. And finally, when she got to hold him again, I could see that the entire world was turned off for her, and there was only she and her son. She wanted and needed nothing else. It made me think of God's attitude toward us, and it filled me with hope and joy and admiration, both for this woman and for God who created her and who created us, and who aches for and loves us each even more desperately than this.
Friday, November 22, 2013
OB/GYN: The Hard Questions
So, this rotation makes me ask all kinds of questions. The first one is the most fundamental. When does life begin? And related to that...
- Should we be mourning miscarriages? Ectopic pregnancies? Vanishing twins? Partial molar pregnancies? Degenerated IVF blastocysts? What about blighted ova?
- Is hormonal contraception ever useable in sexually active women? In any woman of reproductive age?
- Are barriers licit to prevent STD transmission between spouses?
- Is emergency contraception ever useable in victims of rape? Which forms? (Paraguard? Which isn't currently to be given to victims of rape?)
- Is ovarian hyperstimulation licit?
- Is IVF licit?
- When is sterilization okay?
- What should we do for women who shouldn't have more children?
- What is parenthood? Genes, gestational carriers/surrogates, adoptive parents? How should men and women licitly become parents?
Death
 I have not yet seen someone die, although many of my classmates have. I may when I am on inpatient IMED or surgery.
I have not yet seen someone die, although many of my classmates have. I may when I am on inpatient IMED or surgery. I have only seen little signs of death. As I was walking out of the hospital to my car, I once saw a hearse pull up to the building where I know the pathology lab is. I guess the morgue is down there, in the basement. The hearse was pulled up into a place where dumpsters were. That made me sad, that the body of the deceased person was among the trash.
My second brush with death just occured, only a few minutes ago. I'm sitting in the student lounge (I'm supposed to be studying), and a few minutes ago I heard sobbing outside the door. I debated about whether to ignore it, but I went out after a moment and found two women, one weeping and one crying loudly. I asked what was wrong.
The weeping woman wiped her eyes and said, "my brother's back there," pointing to the third-floor ICU located behind the student lounge. After I asked whether I could do anything for them and offered to pray, I went back into the lounge. Twenty or so minutes later (now) I heard new, loud cries from the same place, joined by a man. And I prayed for the man's soul. I don't know if he had died, but he may have. Please pray for the departed of this hospital and all hospitals today!
Tuesday, November 19, 2013
Medical Symbols
According to Aristotle, followed by the Church with St. Thomas, our bodies are the matter informed by our souls. Scott Hahn makes a similar analogy when he says "our bodies are symbols of our souls."
There are a lot of medical conditions that speak volumes about our souls. Here are just a few. (Note: this is never to say that people with these conditions have the analogous spiritual state; some conditions are heritable or acquired by actions whose objective morality no outside person can judge.)
Heterotopic heart transplant
Occasionally, patients with heart failure are candidates for a heterotopic graft. This means that the patient's heart is not removed and a donor heart is hooked up next to it to share the load of pumping. The person has two heartbeats. This can be done in heart failure is due to severe lung disease, or when the patient's heart might recover (at which point the donor heart would be removed, and the person would have one heartbeat again).
You know when you're trying to acquire a virtue, but your heart just isn't in it? You get up when your alarm rings not because you're excited about being disciplined for God or for others, but begrudgingly. You think to yourself, "my emotions aren't aligned with the right thing, my nature is fallen. I'm trying to become virtuous by replacing the wrong thought (snoozing) with the right one (getting up) and whipping up my emotions artificially. Boy, does this feel fake."
Eventually, virtue grows as you acquire the habit of getting up. And eventually, maybe you'll be like Mother Teresa, whose emotions and will were so aligned with God's will (who so had the virtue of charity) that it pained her not to go and help the dying.
But until then, you fake it. Your disease is so severe that your heart can't agree with the right thing to do, and you're attracted to evil. But God helps you with actual grace, pumping you up to be virtuous until your own heart is so transformed into His that it beats in synchrony, and you want the good.
There is one other symbol that I find particularly striking: syphilis. This includes graphic pictures, but no explicit images.
There are a lot of medical conditions that speak volumes about our souls. Here are just a few. (Note: this is never to say that people with these conditions have the analogous spiritual state; some conditions are heritable or acquired by actions whose objective morality no outside person can judge.)
Heterotopic heart transplant
 |
| Donor heart on left; patient's original heart on right. |
You know when you're trying to acquire a virtue, but your heart just isn't in it? You get up when your alarm rings not because you're excited about being disciplined for God or for others, but begrudgingly. You think to yourself, "my emotions aren't aligned with the right thing, my nature is fallen. I'm trying to become virtuous by replacing the wrong thought (snoozing) with the right one (getting up) and whipping up my emotions artificially. Boy, does this feel fake."
Eventually, virtue grows as you acquire the habit of getting up. And eventually, maybe you'll be like Mother Teresa, whose emotions and will were so aligned with God's will (who so had the virtue of charity) that it pained her not to go and help the dying.
But until then, you fake it. Your disease is so severe that your heart can't agree with the right thing to do, and you're attracted to evil. But God helps you with actual grace, pumping you up to be virtuous until your own heart is so transformed into His that it beats in synchrony, and you want the good.
There is one other symbol that I find particularly striking: syphilis. This includes graphic pictures, but no explicit images.
Saturday, November 16, 2013
Happenings in OB/GYN
Two weeks ago I shadowed an OB/GYN who specialized in Reproductive Endocrinology and Infertility (REI). I observed half a dozen discussions about IVF, donor eggs, and donor embryos. And I had a personal tour of the IVF lab. It was surreal and confusing and heartbreaking.
Conception and Death
Last week I was rounding on the gynecology service, and was scheduled to scrub in on a ruptured ectopic pregnancy. The same day, I saw a patient with disseminated ovarian cancer who was being "withdrawn" from aggressive ICU care (heroic measures were stopped and she was allowed to die naturally only a few minutes after I listened to her heart and lungs). The beginning and the end of life, in one day.
Numbers
I have now been to 3 vaginal births and 5 C-sections (one of which was for twins). There was one C-section for prolonged rupture of membranes and severe intrauterine infection. The amniotic fluid gushed a thick purple, like blueberry syrup at IHOP, instead of a healthy clear. The inside of the uterus was mushy and white, instead of the typical mossy red. The baby was a preemie in frank breech, and the NICU team took him and (again, not as usual) didn't bring him back to the Mom before the procedure ended. I hope they do well.
Minefield
I ended up not scrubbing on that ectopic pregnancy case, but it created a small stir for me. When I was told I was scheduled to do it, I thought, "oh great! I am especially interested in ectopic pregnancy and tubal surgery!" This is I want to save early lives and give couples with tubal factor infertility an option besides IVF! Then I realized, "oh dear. What if the surgery planned is a salpingostomy, or salpingotomy?" Quickly, I looked at the patients records and saw that she was planned for salpingectomy. I breathed a sigh of relief.
No such relief for a recent C-section with post-partum tubal ligation. I was scrubbed in on a C-section and then discovered that the patient and her surgeon were planning sterilization. Now normally, it is the medical student's job to stand at the operating table and do menial tasks, such as holding retractors, suctioning, and dabbing the field with lap sponges. Perhaps the best of these menial tasks is cutting suture. For this task, I actually need to ask for an instrument from the scrub tech. "Suture scissors," I say, and hold out a hand. She slaps the plain-jane scissors into my palm, and I proudly cut the ends of the residents' or attendings' thread. A medical student is slacking or inattentive if someone else calls for the suture scissors.
For the tubal ligation, which involves cutting of four sutures, I folded my hands and stood at the table, simply observing and listening. I pretended to be forgetful of asking for the scissors. Once that procedure was done, though, I resumed cutting, retracting, and sponging for the rest of the C-section.
Call
I had my first night call last week. I worked a typical day on gynecology (I got to work at 4:50am for rounds at 6:00), and then had a dinner break from 5:00pm to 5:45pm, at which point I worked until about 7:30 the next morning, with a 45-minute nap somewhere in between. That was exhausting. I am not sure I've stayed up for 24 hours before that. Ever. And I've got to do that again tomorrow. Merp.
Overall, OB/GYN is good.
I like the clinic, I like the surgery, and I love deliveries. I don't like all the people I'm working with, and I don't like knowing so little about what I want to do. It's a little stressful, but overall I'm enjoying it. One thing I'm struggling with is how prayer fits in to a 60-hour work week. During the past week, I've been paging the hospital chaplain and receiving communion from him on days I can (and that means I missed two days!), and I've missed parts of the Liturgy of the Hours several times. Even so, I think I am doing God's will, and I have fewer occasions of sin, and my thoughts stray to Jesus more easily.
Sunday, November 3, 2013
Two quick stories
I have to go to Mass in a few minutes, but I really wanted to squeak out a post.
At the end of my pediatrics rotation, a patient came in with a "hurt arm." I examined her and though we needed an elbow radiograph to rule out fracture (although I told the doc I thought it was a soft tissue injury, since she had so point tenderness). She got an X-ray and came back after hours (I stayed!) and we read the film. I saw something we had just learned about in radiology lectures, and said "isn't that a posterior fat pad sign?" Brownie points for that!
As the doctor was explaining the diagnosis to the parents (supracondylar fracture) the mother began to pale and she actually fainted. We laid her down on the examination table and the MA got her some cherry pedialyte and goldfish when she woke up. Then we put a splint on her daughter and the three of them went home. So, that was a terribly told story but that's what happened!
Story #1
At the end of my pediatrics rotation, a patient came in with a "hurt arm." I examined her and though we needed an elbow radiograph to rule out fracture (although I told the doc I thought it was a soft tissue injury, since she had so point tenderness). She got an X-ray and came back after hours (I stayed!) and we read the film. I saw something we had just learned about in radiology lectures, and said "isn't that a posterior fat pad sign?" Brownie points for that!
As the doctor was explaining the diagnosis to the parents (supracondylar fracture) the mother began to pale and she actually fainted. We laid her down on the examination table and the MA got her some cherry pedialyte and goldfish when she woke up. Then we put a splint on her daughter and the three of them went home. So, that was a terribly told story but that's what happened!
Story #2
At the beginning of my OB/GYN rotation, I was working in the private practice of a local OB/GYN and one of her patients came in for "rule out labor" (i.e. she was having contractions and wanted to know if she should go to the hospital). The answer (after we hooked her up to a fetal cardiac monitor, looked at the strip, and examined her cervic was yes, you are four centimeters and go now. The physician called the hospital ahead of time.
A few patient visits later, the phone rang for the doctor and her eyes widened as she listened. She slammed the phone down after a quick "thank you," and said to me, "that patient's complete" (meaning, she's dilated to 10 centimeters and is ready to push). The doctor said to me, "you'd better leave now, because I'm going straight there after I finish this chart, and I'm going to fly."
I raced to the hospital through the molasses of midafternoon traffic and jumped into a pair of scrubs. I didn't have appropriate shoes, but I slipped boot covers over my pumps. I helped with the delivery (at one point only I and the L&D nurse were in the room as she pushed!) and delivered the placenta. My first delivery in high heels (and hopefully the last).
Monday, October 21, 2013
I Wish I'd Known
| Prayer will make you beautiful! It might not give you flowing dark hair, though. Sad face. |
I've thought about this several times recently: I listened to a talk from the School of Faith (get the talk by creating a login here; it's Faith Foundations I Lesson 9) and I read this post about prioritizing prayer and then I heard my parish priest give a homily saying pretty much the same thing just yesterday.
Do you live an age-appropriate prayer life? This article might be a good help towards a beginning to grow up into spiritual adolescence. And asking someone who is a little further along in the journey was helpful for me; hopefully God will (or has already) placed this person in your life. If not, pray that He will!
Now you know what I wish I'd known. God bless you today!
Tuesday, October 15, 2013
What is formation like for consecrated virginity?
Disclaimer: you are now reading a post about formation by the one being formed, not by the formers, which is kind of like asking a second-grader about the objectives and milestones required to advance to the third grade. </disclaimer>
Formation for consecrated life is formation for the whole person, to prepare them to live as a spouse of Christ on earth and a mother of souls. Forming the whole person includes spiritual, intellectual, and affective components. For example, I am taking a Faith Foundations class through the School of Faith (it's free and available to you, too!) for intellectual formation right now. For affective and spiritual formation, I am following a rule of life and meeting with local focolarine weekly. Each week, we review and share on practical applications of topics like:
Formation has been challenging but amazing. I am shocked at the changes I see in myself just in the past 12 weeks. The most important part has been having spiritual mothers to set an example of unconditional love. God is radiantly generous!
Formation for consecrated life is formation for the whole person, to prepare them to live as a spouse of Christ on earth and a mother of souls. Forming the whole person includes spiritual, intellectual, and affective components. For example, I am taking a Faith Foundations class through the School of Faith (it's free and available to you, too!) for intellectual formation right now. For affective and spiritual formation, I am following a rule of life and meeting with local focolarine weekly. Each week, we review and share on practical applications of topics like:
- God loves me immensely (where? when last week? even when you were suffering? how do you know? do you trust Him?)
- doing God's will in the present moment (even in the car? are you patient in the present moment? do you stay there with Him?)
- loving like God: first, unconditionally, with a smile (this is how you spend the whole day with Him! If only I knew anything about it....)
- the Word of God lived out in life (we're on this now and I'm totally confused)
Formation has been challenging but amazing. I am shocked at the changes I see in myself just in the past 12 weeks. The most important part has been having spiritual mothers to set an example of unconditional love. God is radiantly generous!
Academic Medicine 101
Before I started medical school, I had no idea that "academic medicine" is the segment of medicine that researches and teaches. Some physicians see patients all day, every day while others do research (either clinical, basic, or translational) or teach (e.g. lecture, and supervise the practice of residents and the visits and notes of medical students rounding under them). Most of my experience of academic medicine is with the teaching physicians. Let me tell you about it.
First of all, I haven't had my big academic rotation yet. This is the famous "Internal Medicine" rotation (shortened in speech to "IM" for some schools, "I-Med" for us). From what I hear, that is twelve of the most intense weeks of seeing patients, giving presentations, writing notes, being humiliated, and learning the minute mechanics of fluid and medical management.
Did you catch the "being humiliated" in there?
Although I haven't had IMed (and so I feel like I can't really talk about this?), I have had one week of adult inpatient and one week of pediatric inpatient. My attending last week (pediatric) literally said that medicine is taught by shame. "That's how you remember things," he said, "by being put on the spot." I like to think that it's not shame, but responsibility that teaches us. When a person in need, in front of you, is your patient and your attending asks you "how are you going to replace his potassium in light of his serum creatinine?" and you blanch and have no clue, you're going to learn it well and know it next time.
Last week, for instance, I had one week of pediatrics. I got up early to report to the hospital an hour before the attending scheduled "rounds." I was assigned one patient each day, and went to talk with them and examine them and prepare a presentation and admission orders, including IV fluids, drugs and doses, and special nursing instructions. (All of these orders were practice; none were actually carried out except if someone else, e.g. the resident or fourth year, had the same idea/agreed with me and ordered them.)
"Rounds" is when the attending physician (the doctor in the leadership chair, over the third- and fourth-year medical students and residents on the "team") and the lowerlings meet to review everyone's work. Last week, there were three third-year students, one fourth-year (doing an elective in peds, his specialty choice), and a family medicine resident (doing a rotation in peds), along with a pharmacy student (?) and a recently-hired NP (rounding to get the feel of the unit, I guess) followed the attending from room to room. At each room, the lowliest person who'd seen the patient would present them. Each of the third-years saw one patient, the fourth year saw two or three, the resident saw almost all the patients, and the attending was responsible for all of them. This means that the patient I saw was seen by the fourth-year (sometimes) and the resident (frequently), so that when my presentation was over that person would add findings, challenge me, or critique my plan (instead of the attending).
When we came to my patient's room, the attending would face me and say, "go," or I would make eye contact with him and start presenting. "This is a 13-month-old white female who presents with a four-day history of vomiting," I'd rattle off. I'd then describe the history of the present illness (HPI), the pertinent positives and negatives, past medical/surgical history (including birth history for children!), currents meds and allergies, and my objective findings (vital signs, physical exam, labs, and imaging). Then, I state my assessment and plan. "This is a 13-month-old female with gastroenteritis. Plan is replace fluid losses with D5 one-half normal and attempt p.o. challenge today."
And then the education would begin. The attending critiques your presentation skills (if you're really new at this), asks for additional findings (and you better hope you have them), and corrects your plan (you feel awesome if this is all he has to say). Since I am new to this, I got lots of presentation-skills and additional-findings criticism.
Presentation skills are important because we're in medical school to learn to think in an orderly, analytical way about complex problems and not miss things. We're trained to think like a doctor by presenting and writing notes. Presenting skills are also important because communication to colleagues is made quick and safe by a universally-agreed upon format. The format in medicine is:
If your attending asks for additional findings, you are expected to produce them with ease. It looks sort of silly to shuffle through your papers, although that's better than having to say "I don't know" or "I didn't ask." We are supposed to know everything about our patients. (Was there green in the vomit? How far did it fly? What was her serum chloride on Monday? Did we get the results of the 99-technetium scan?) Not knowing a historical detail is not very excusable (it's a rookie mistake, only one level above the presentation skills problems); not knowing a lab result is only slightly less excusable. And one is looked upon as not up to snuff if you miss out on a social issue (e.g. illiteracy, bad home situation, poverty, mental illness, etc).
And A/P criticism, while desired, comes in very different flavors. "I think you forgot a decimal point on her IV fluids" is a lot better than "Now, if you give this potassium, you'll probably put this guy into acute kidney failure. You want that on your hands?" But even so, this is the best tier of criticism, and one hopes to reach it during every presentation.
One problem in this approach is stressed or nervous med students, or those who are shy or have thin skins or fragile self esteem, can get hurt. One girl last week cried! I have been lucky, since TAC and high school accustomed me to faking it till I make it (in terms of confidence, not A/Ps). I also have a good memory for medical knowledge. But I don't like that some med students have to learn by shame and embarrassment. I wish we could all take on responsibilities without being toughened by humiliation. Stay tuned for more about academic medicine in the spring, when I go "on the wards" for twelve weeks of I-Med.
First of all, I haven't had my big academic rotation yet. This is the famous "Internal Medicine" rotation (shortened in speech to "IM" for some schools, "I-Med" for us). From what I hear, that is twelve of the most intense weeks of seeing patients, giving presentations, writing notes, being humiliated, and learning the minute mechanics of fluid and medical management.
Did you catch the "being humiliated" in there?
Although I haven't had IMed (and so I feel like I can't really talk about this?), I have had one week of adult inpatient and one week of pediatric inpatient. My attending last week (pediatric) literally said that medicine is taught by shame. "That's how you remember things," he said, "by being put on the spot." I like to think that it's not shame, but responsibility that teaches us. When a person in need, in front of you, is your patient and your attending asks you "how are you going to replace his potassium in light of his serum creatinine?" and you blanch and have no clue, you're going to learn it well and know it next time.
Last week, for instance, I had one week of pediatrics. I got up early to report to the hospital an hour before the attending scheduled "rounds." I was assigned one patient each day, and went to talk with them and examine them and prepare a presentation and admission orders, including IV fluids, drugs and doses, and special nursing instructions. (All of these orders were practice; none were actually carried out except if someone else, e.g. the resident or fourth year, had the same idea/agreed with me and ordered them.)
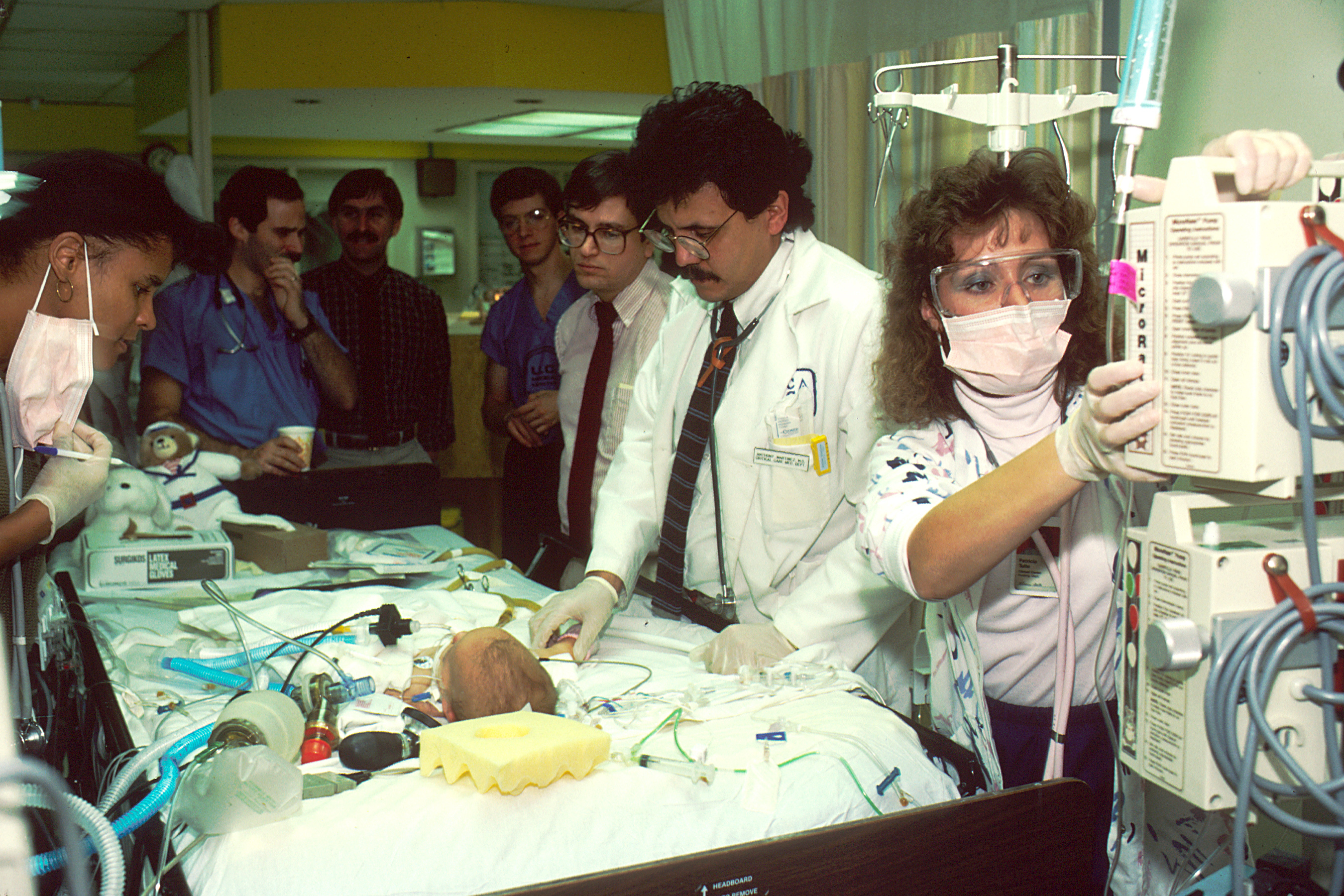 |
| All the people standing behind the attending (who is actually examining the patient) are the med students, etc. A nurse happens to be adjusting the IV fluids at the same time. |
When we came to my patient's room, the attending would face me and say, "go," or I would make eye contact with him and start presenting. "This is a 13-month-old white female who presents with a four-day history of vomiting," I'd rattle off. I'd then describe the history of the present illness (HPI), the pertinent positives and negatives, past medical/surgical history (including birth history for children!), currents meds and allergies, and my objective findings (vital signs, physical exam, labs, and imaging). Then, I state my assessment and plan. "This is a 13-month-old female with gastroenteritis. Plan is replace fluid losses with D5 one-half normal and attempt p.o. challenge today."
And then the education would begin. The attending critiques your presentation skills (if you're really new at this), asks for additional findings (and you better hope you have them), and corrects your plan (you feel awesome if this is all he has to say). Since I am new to this, I got lots of presentation-skills and additional-findings criticism.
Presentation skills are important because we're in medical school to learn to think in an orderly, analytical way about complex problems and not miss things. We're trained to think like a doctor by presenting and writing notes. Presenting skills are also important because communication to colleagues is made quick and safe by a universally-agreed upon format. The format in medicine is:
- Patient ID sentence
- Chief concern
- HPI
- Review of systems (ROS)
- Past medical history (including birth history if pediatrics)
- Past surgical history
- Current meds
- Family history
- Social history
- Allergies
- Vital signs
- Physical exam
- Labs
- Imaging
- Assessment/Plan (A/P)
If your attending asks for additional findings, you are expected to produce them with ease. It looks sort of silly to shuffle through your papers, although that's better than having to say "I don't know" or "I didn't ask." We are supposed to know everything about our patients. (Was there green in the vomit? How far did it fly? What was her serum chloride on Monday? Did we get the results of the 99-technetium scan?) Not knowing a historical detail is not very excusable (it's a rookie mistake, only one level above the presentation skills problems); not knowing a lab result is only slightly less excusable. And one is looked upon as not up to snuff if you miss out on a social issue (e.g. illiteracy, bad home situation, poverty, mental illness, etc).
And A/P criticism, while desired, comes in very different flavors. "I think you forgot a decimal point on her IV fluids" is a lot better than "Now, if you give this potassium, you'll probably put this guy into acute kidney failure. You want that on your hands?" But even so, this is the best tier of criticism, and one hopes to reach it during every presentation.
One problem in this approach is stressed or nervous med students, or those who are shy or have thin skins or fragile self esteem, can get hurt. One girl last week cried! I have been lucky, since TAC and high school accustomed me to faking it till I make it (in terms of confidence, not A/Ps). I also have a good memory for medical knowledge. But I don't like that some med students have to learn by shame and embarrassment. I wish we could all take on responsibilities without being toughened by humiliation. Stay tuned for more about academic medicine in the spring, when I go "on the wards" for twelve weeks of I-Med.
Saturday, October 12, 2013
Aaaaand...pie.
 It's been forever since I put some cooking stuff up here! Last Saturday I and my sister made an apple pie. It was beautiful! We cut the apple logo into the hand-made top crust, but I didn't take a picture until it was mostly eaten. I guess that's a testament to how good it was!
It's been forever since I put some cooking stuff up here! Last Saturday I and my sister made an apple pie. It was beautiful! We cut the apple logo into the hand-made top crust, but I didn't take a picture until it was mostly eaten. I guess that's a testament to how good it was!Winter is coming, and I hope that means more pies in the future. I've got plans for pumpkin, peach-and-blackberry, cherry, pecan, and strawberry-and-rhubarb.
 |
| Right before the oldest brother snarfed the rest of it. |
Monday, October 7, 2013
Lacey's Story
 While working at the psychiatric hospital in admitting, I was sent to speak with Lacey, a girl who came in with her mother. It was up to me to fill out the interview form, do the mental status exam, and decide whether the girl would be admitted to the mental hospital or not. Of course, I would present the case to my attending, who would check my work and (hopefully) catch my mistake, but I still felt like I was being handed a lot of responsibility.
While working at the psychiatric hospital in admitting, I was sent to speak with Lacey, a girl who came in with her mother. It was up to me to fill out the interview form, do the mental status exam, and decide whether the girl would be admitted to the mental hospital or not. Of course, I would present the case to my attending, who would check my work and (hopefully) catch my mistake, but I still felt like I was being handed a lot of responsibility.I went to the waiting room and called the girl's name. A middle-school-aged girl and a young woman, baby on hip, stood and followed me to a room. After introductions, I asked Lacey what brought her in. She did not answer, but only looked out the window, away from me. His mother began to speak, and told me a long and convoluted story about marijuana, bad crowds, running away, and fights.
As the mother spoke, I looked at Lacey, who skillfully avoided eye contact with everyone. I had just finished two weeks on the alcohol and drug dependence ward, and so my soul was full of stories that began like Lacey's and ended with hard street drugs, divorces, dead loved ones, and dead dreams. I looked at her and wondered: will you go down one of those paths, or is this just a slightly-more-serious-case of teenage rebellion? And another possibility: is your mom the crazy one? She's the one doing all the talking.
The baby had fallen asleep on Lacey's mother's chest by the time the story was finished.
"Thank you so much for helping me understand," I told her. "I know it's been a long wait for you, but would you mind stepping out so that I can talk to Lacey?"
 She left, and I turned to the silent teenager in front of me. She still gazed out the window. Was that a grave silence or a nonchalant silence or a hurt silence or a panicked silence or...?
She left, and I turned to the silent teenager in front of me. She still gazed out the window. Was that a grave silence or a nonchalant silence or a hurt silence or a panicked silence or...?"Lacey," I said, "I want to hear your side of the story."
Nothing.
"What your mom told me...does that match what happened?"
Nothing. I tried one or two more times. Still nothing.
"Well," I said, taking a new tack, "pardon me while I fill out some paperwork." And so I sat there, across the table from her, checking boxes on the mental status exam. I wanted to show her I wasn't afraid of silence. Several minutes passed.
"You know," I said at last, trying to speak like one seventh-grader to another (or one medical student to another), "I can't make you stay. Finally, you decide whether we can help you or not. Do you think you need help? Do you want to stay?"
A few more seconds of nothing, then Lacey's eyes moved from the window to his lap. Then she nodded. My heart soared, partially with elation at successfully communicating and partially because I thought she really could use the help.
"Okay," I said softly. I didn't follow Lacey after this, but I won't forget this interview soon. Pray for her if you read this.
Saturday, October 5, 2013
Pediatrics: An Inspiring Rotation
Although pediatrics has not felt as relevant as other rotations, I've certainly had a lot of chances to be humbled and amazed by the parents I meet.
During the physical exam, however, the doctor had to palpate for swelling and tenderness to palpation (an X-ray was inconclusive), and the pain began to be more than Aaron could communicate. Unable to say "stop it" fast enough, he screamed loudly, then began to cry. The doctor stopped and we stepped out of the room for a time, while Aaron and his mother re-grouped.
After a few minutes, we came back in. "Aaron wants you to know he's embarrassed," his mother said gently, "but he wasn't prepared for you doing that today." The doctor nodded, apologized to Aaron, and the interview went on. It reminded me of a video I'd seen about a nonverbal girl with autism (at right and also online: Carly's Cafe). It was as if Aaron's world was too overwhelming, and processing it took so much time that he couldn't ask the doctor to stop pressing, and the pain and the inability to stop it became very distressing.
Throughout, the mom was a calm and loving help to this young man who she was barely helping to function. At one point in the interview, she became tearful when she talked about Aaron "falling through the cracks." Where would Aaron be without this woman? This is another story of someone I'll not forget easily, someone whose generosity was humbling.
"Lupita"
In the outpatient clinic I worked in, my preceptor had me shadow for well child visits. One afternoon, I followed him into a well child check, only to see no child in the room...only a middle-aged woman sitting in the corner chair. She and the pediatrician began to speak and I slowly began to understand what was going on.
This woman was adopting a distant relative's child, "Lupita" after discovering that Lupita and her siblings were being neglected. Raised in a small town in south Texas, the children were left alone often and had to choose which children ate at meals. Lupita didn't speak English very well and didn't know what grade she was in. The woman said that at home, Lupita talked nonstop to whoever was around her and ate voraciously, almost choking on a sandwich in her haste to eat it. Drug use and deportation played a role in her mother's absence.
Lupita came in after the pediatrician had received all this news. She was a grave child, obeying the doctor in everything she could understand without smiling or showing any embarrassment that a girl her age would typically show. She spoke freely but only when spoken to. In her hand, she held a little charm, and when I asked her what it was, she opened her hand and showed me a plastic star the size of a die. "Mi estrella," she said simply.
I was very amazed by Lupita's new adoptive mother. This woman was also planning to adopt Lupita's baby brother, who was still in Mexico. And when my preceptor asked, "how do your twins feel about all this?" I was completely amazed. Pray for them!
"Aaron"
In the same outpatient office, with a different preceptor, I saw a follow-up with eighteen-year-old "Aaron" on a stress fracture. Aaron was a young adult with autism and a lot of sensory overload. He was in a post-high school program designed to teach adults to ride public transport, interview for a job, and use a basic skill set in an employment setting. He had come in with his mother, who I learned (and could see by difference in race) was his adoptive mom.
As the doctor conducted the history from his mother, Aaron would constantly interrupt: "what's going on? I don't understand," or "I have something to say. I'm going to explode. I still don't understand," and his mother would quietly redirect him or ask him for input. She was very skillful at letting Aaron talk as much and as constructively as possible, while also advancing the discussion of his painful foot.
As the doctor conducted the history from his mother, Aaron would constantly interrupt: "what's going on? I don't understand," or "I have something to say. I'm going to explode. I still don't understand," and his mother would quietly redirect him or ask him for input. She was very skillful at letting Aaron talk as much and as constructively as possible, while also advancing the discussion of his painful foot.
During the physical exam, however, the doctor had to palpate for swelling and tenderness to palpation (an X-ray was inconclusive), and the pain began to be more than Aaron could communicate. Unable to say "stop it" fast enough, he screamed loudly, then began to cry. The doctor stopped and we stepped out of the room for a time, while Aaron and his mother re-grouped.
Throughout, the mom was a calm and loving help to this young man who she was barely helping to function. At one point in the interview, she became tearful when she talked about Aaron "falling through the cracks." Where would Aaron be without this woman? This is another story of someone I'll not forget easily, someone whose generosity was humbling.
"Helen"
I just finished the week of newborn nursery time that's sandwiched between the other weeks of pediatrics. I rotated through the NICU and saw some very incredible moms there, too. I spent some time talking with one in particular, "Helen," who had delivered two preemies. Her first child was born at 28 weeks and she spent months in the NICU fighting lung problems and sepsis. While her baby used IVs and NG tubes, Helen pumped breastmilk from the day he was born, hoping that when he was mature enough he could take it. It was a nightmare, she said, something "I wouldn't wish on anyone." Fortunately, her son is now caught up in growth and milestones, and has no residual CNS effects except some possible learning disability.
During her second pregnancy, Helen received weekly progesterone injections (thick, oily, slow gluteal IM shots) and underwent cerclage, but still went into labor at 28 weeks. After trying every drug her MFM had to offer, she started a terbutaline drip at home and stayed on bedrest for six weeks. Helen told me she has a propensity to contact dermatitis and the indwelling needle for the terbutaline drip was a constant irritant in her leg during that month and a half. And at some point every week, she would go into labor again and the terbutaline dose would have to be increased in the emergency room.
"Was it worth it?" I asked.
"Oh, absolutely," Helen said emphatically. "My daughter was born at 36 weeks, and it was so worth it to have her that much farther along. Oh, absolutely." This woman has her priorities in beautiful order. The generosity of soul of these mothers astounds and humbles me!
During her second pregnancy, Helen received weekly progesterone injections (thick, oily, slow gluteal IM shots) and underwent cerclage, but still went into labor at 28 weeks. After trying every drug her MFM had to offer, she started a terbutaline drip at home and stayed on bedrest for six weeks. Helen told me she has a propensity to contact dermatitis and the indwelling needle for the terbutaline drip was a constant irritant in her leg during that month and a half. And at some point every week, she would go into labor again and the terbutaline dose would have to be increased in the emergency room.
"Was it worth it?" I asked.
"Oh, absolutely," Helen said emphatically. "My daughter was born at 36 weeks, and it was so worth it to have her that much farther along. Oh, absolutely." This woman has her priorities in beautiful order. The generosity of soul of these mothers astounds and humbles me!
Thursday, October 3, 2013
How to Discern whether You should Become a Doctor
Our healthcare system is changing. If you know a young student thinking about medical careers, help them
make an informed decision about what type of medical professional they should become.
First of all, think outside the box: not all medical careers have to be preceded by getting MDs, DOs, PAs, or RNs. If you like the operating room, consider becoming an OR tech. If you love children, think about becoming a child life specialist. If you like the intensity of the ICU or EMS, try respiratory therapy or becoming an EMT. If you love helping people and have another special talent, think about music therapy, speech therapy, pet therapy, or occupational therapy. If you love sports or movement, try physical therapy or massage therapy. If you want to work with the elderly, consider LVN and hospice or nursing home work. If you like chemistry, think about becoming a med tech, a lab tech, pharm tech, or getting a PharmD. And if you like ambulatory medical care that is flexible enough for a family, consider dentistry or dental hygiene. Phlebotomy (including dialysis and donor), medical assisting, billing, hospital or practice administration...there are many medical careers that require various gifts. At the beginning of your thought process, use your imagination to try on a wide variety of careers and ask people in those careers what else they thought about.
Now, let's talk about MDs, DOs, PAs, and RNs. A person with one of these degrees can choose from a wide variety of practices at the completion of their degree. For instance, MDs and DOs ("doctors" or "physicians") can become primary care doctors (for children, adults, or both), specialists (in a particular time of life, like geriatricians or obstetricians; or for a particular organ system, like cardiologists and endocrinologists; or for a particular disease, like oncologists). PAs ("physician assistants") can do almost anything doctors do, from surgery to private practice. RNs ("nurses") work in all kinds of settings as well, especially inpatient settings like nursing homes, adult/pediatric/obstetric hospitals, surgical settings, ICUs, PACUs, NICUs.... Some RNs work call centers, which is a good option for those who want to work from home and have a family. RNs can also become nurse practitioners (NPs), which enables them to take on the responsibilities of a clinician.
Let's clarify the word "clinician." A clinician is a person who physically examines patients, diagnoses their conditions, and prescribes a treatment plan. Unlike a technician who may perform specific tests (like measuring blood pressure, taking an X-ray, measuring an ABI, or performing an ultrasound), a clinician is responsible for combining the results of tests with findings from his physical exam to create a plan of care and manage that plan. Doctors, PAs, and NPs can all do this. PAs and NPs (sometimes called "mid-levels") require a physician's supervision, but this is very loose when the relationship is established and the mid-level's experience is solid.
Our healthcare system is changing, and the rise of mid-levels is a sign of this change. A mid-level can do now what a doctor did in the early last century; a doctor now has a different set of unique privileges. So why become a physician when you can examine, diagnose, prescribe, and manage patients as a PA or NP? What's unique about becoming a physician?
A physician (MD or DO) is, in addition to being a clinician, a supervisor of clinicians. In addition, he can be an entrepreneur (e.g. starting a practice, group, clinic, or even hospital) with greater ease and independence than a mid-level or other healthcare worker. Moreover, he can be an innovator: his depth of education (somewhere between the mid-level and a Ph.D. in several subjects) allows him to design new therapies for patients and legally try them. Finally, he can subspecialize or superspecialize: as an example, I could become an OB/GYN and then do a fellowship in maternal-fetal medicine or a fellowship in naprotechnology. If I start a clinic I can employ other physicians or mid-levels who practice general OB or general GYN, while I care for high-risk women or complicated surgical cases. In conclusion: in our day and age, the MD or DO is the highest degree in medical careers enables a person to be a supervisor, entrepreneur, innovator, and subspecialist. If you don't want to be one or more of these things, I suggest going mid-level: you'll still have your patients, you'll still diagnose and manage, but you won't have as many years of school, nor as much debt and liability!
I hope this is a helpful tool for anyone considering a medical career. I see that some of my classmates have the wrong reasons for becoming a physician, and others are fatigued by the amount of school. I don't want this to happen to you (or the person you think could read this and find it helpful), so I encourage you to think and pray about this carefully. Finally, thank you for considering a medical career: it's a corporal work of mercy and an extremely fulfilling path. Whatever you choose to do, I hope you enjoy it!
 |
| Child life specialist. |
Now, let's talk about MDs, DOs, PAs, and RNs. A person with one of these degrees can choose from a wide variety of practices at the completion of their degree. For instance, MDs and DOs ("doctors" or "physicians") can become primary care doctors (for children, adults, or both), specialists (in a particular time of life, like geriatricians or obstetricians; or for a particular organ system, like cardiologists and endocrinologists; or for a particular disease, like oncologists). PAs ("physician assistants") can do almost anything doctors do, from surgery to private practice. RNs ("nurses") work in all kinds of settings as well, especially inpatient settings like nursing homes, adult/pediatric/obstetric hospitals, surgical settings, ICUs, PACUs, NICUs.... Some RNs work call centers, which is a good option for those who want to work from home and have a family. RNs can also become nurse practitioners (NPs), which enables them to take on the responsibilities of a clinician.
Let's clarify the word "clinician." A clinician is a person who physically examines patients, diagnoses their conditions, and prescribes a treatment plan. Unlike a technician who may perform specific tests (like measuring blood pressure, taking an X-ray, measuring an ABI, or performing an ultrasound), a clinician is responsible for combining the results of tests with findings from his physical exam to create a plan of care and manage that plan. Doctors, PAs, and NPs can all do this. PAs and NPs (sometimes called "mid-levels") require a physician's supervision, but this is very loose when the relationship is established and the mid-level's experience is solid.
Our healthcare system is changing, and the rise of mid-levels is a sign of this change. A mid-level can do now what a doctor did in the early last century; a doctor now has a different set of unique privileges. So why become a physician when you can examine, diagnose, prescribe, and manage patients as a PA or NP? What's unique about becoming a physician?
A physician (MD or DO) is, in addition to being a clinician, a supervisor of clinicians. In addition, he can be an entrepreneur (e.g. starting a practice, group, clinic, or even hospital) with greater ease and independence than a mid-level or other healthcare worker. Moreover, he can be an innovator: his depth of education (somewhere between the mid-level and a Ph.D. in several subjects) allows him to design new therapies for patients and legally try them. Finally, he can subspecialize or superspecialize: as an example, I could become an OB/GYN and then do a fellowship in maternal-fetal medicine or a fellowship in naprotechnology. If I start a clinic I can employ other physicians or mid-levels who practice general OB or general GYN, while I care for high-risk women or complicated surgical cases. In conclusion: in our day and age, the MD or DO is the highest degree in medical careers enables a person to be a supervisor, entrepreneur, innovator, and subspecialist. If you don't want to be one or more of these things, I suggest going mid-level: you'll still have your patients, you'll still diagnose and manage, but you won't have as many years of school, nor as much debt and liability!
I hope this is a helpful tool for anyone considering a medical career. I see that some of my classmates have the wrong reasons for becoming a physician, and others are fatigued by the amount of school. I don't want this to happen to you (or the person you think could read this and find it helpful), so I encourage you to think and pray about this carefully. Finally, thank you for considering a medical career: it's a corporal work of mercy and an extremely fulfilling path. Whatever you choose to do, I hope you enjoy it!
Sunday, September 22, 2013
Mass for the Primitive Pagans Today
I recently went to Mass in a Christian community emerging from a pretty entrenched pagan culture. It was primitive and there were some (less than Christian) parts of the culture that shone through in their particular celebration of the Mass...but on the whole it was actually pretty beautiful to see that many of them were using the faith to christen their culture, themselves, and their children.
Mass was in the vernacular with a few Latin parts (just Agnus Dei, actually). I admire these people for learning even little bits of a language that must seem totally foreign to them.
The church building was no classic European cathedral, that's for sure! I would criticize them for their very mediocre architecture, but that probably wouldn't be fair to the people actually worshipping in the space. They probably don't have as rich a patrimony as Michelangelo! So yes, the Church was all brown and plain, but that's not the most important thing, no?
The music....well, it was no Gregorian chant. There was quite a bit of percussion with instruments native to the people, as well as some strings and lots of voice. It's very important to this society that each person has an equal dignity, so everyone in the congregation sings and says as much as possible in the Mass (they might have stuck in an extra "Amen" in the Eucharistic prayer?). This includes the hymns, so sometimes quality is sacrificed for participation. Theologically, there's better stuff (Adoro Te, Christus Vincit, O Sacred Head are some favs of mine) and even musically, there's better stuff, but they use hymns written by their people and I think they might be better for it, at least until they grow into the Chuch's rich musical heritage.
The people sit in family units, which I think has to do with this culture's historical foundation on the family in agriculture. Or maybe they sit in family units just because they travel to Mass that way from home. Who knows! But either way, it's a quiet and helpful way to reinforce the sacredness of the family.
Also of note, they exchange an already culturally-established sign of peace. (I've also seen a Korean community give peace by bowing. That was really fun. Do Europeans kiss?) They also do this at the Our Father with their neighbors, even though it isn't in the Ritual. Is this bad? Not sure...you could argue that they're adding to the Mass, which not even priests should do, but you could also arguing that they're Christianizing an otherwise secular gesture.
There is a great understanding of the sacredness of space in this culture, so it's natural for them to have LOTS of space between the people and the altar, and for this to be totally cool. (In contrast, some Africans or Hispanic cultures love to go right up to tabernacles and monstrances to touch and pray.) Here, there's a definite "holy of holies" and something untouchable about the Blessed Sacrament. That attitude in their culture (that everyone has their space and you don't trespass) is probably from their history, but it's serving them well at Mass!
Everyone is quiet during the homily. Academic achievement is prized in this culture, and I suppose that's probably helping them. On the other hand, they love partying, so perhaps a third of them are dozing off or distracted, bored. I wonder which one will win out as this little community continues in faith!
Hmm, there are female altar servers and women on the altar. Don't get me wrong, I love women. But I don't think this culture has a huge understanding of priestly celibacy and the otherness of Holy Orders as alter Christus capitis. There hasn't been much interest amongst the young men in vocations to the priesthood, either. Could it be that the female presence on the altar is a sign or symptom of this misunderstanding? I hope the gentle teaching of the Church can help the whole community understand the value of celibacy and the value and uniqueness of the priesthood.
Although there is much singing during the Communion of the faithful, almost everyone is reverent. There is no altar rail in this church and the people mostly receive in the hand, although some receive on the tongue while standing. Almost everyone receives communion. Maybe this is a childlike trust; possibly, some are receiving our Lord unworthily, but who am I to judge? I leave it in the hands of the pastor of this young little flock. There was a great deal of singing (even by the people) after all had received--which is not ideal, since some moments of silent communion are appropriate with the Divine Guest--but this is a child's form of prayer, so that might be the intention and the best thing to do. Some of the people abstained from singing and were silent.
After Mass, there was an enormous hubbub as everyone talked about life, children, schools, activities, and everything else. What a vibrant community! There are flowers at statues of our Lady, the Sacred Heart, St. Joseph, and St. Anthony. I think I'll go back soon.
This might not come as a shock to you, but I am describing my home parish in the post-Christian west. Does your home parish impress you when conceived of as a small and newly-converted community in a deeply pagan culture? In some ways, that is what we are. So two pieces of advice:
Mass was in the vernacular with a few Latin parts (just Agnus Dei, actually). I admire these people for learning even little bits of a language that must seem totally foreign to them.
The church building was no classic European cathedral, that's for sure! I would criticize them for their very mediocre architecture, but that probably wouldn't be fair to the people actually worshipping in the space. They probably don't have as rich a patrimony as Michelangelo! So yes, the Church was all brown and plain, but that's not the most important thing, no?
The music....well, it was no Gregorian chant. There was quite a bit of percussion with instruments native to the people, as well as some strings and lots of voice. It's very important to this society that each person has an equal dignity, so everyone in the congregation sings and says as much as possible in the Mass (they might have stuck in an extra "Amen" in the Eucharistic prayer?). This includes the hymns, so sometimes quality is sacrificed for participation. Theologically, there's better stuff (Adoro Te, Christus Vincit, O Sacred Head are some favs of mine) and even musically, there's better stuff, but they use hymns written by their people and I think they might be better for it, at least until they grow into the Chuch's rich musical heritage.
The people sit in family units, which I think has to do with this culture's historical foundation on the family in agriculture. Or maybe they sit in family units just because they travel to Mass that way from home. Who knows! But either way, it's a quiet and helpful way to reinforce the sacredness of the family.
Also of note, they exchange an already culturally-established sign of peace. (I've also seen a Korean community give peace by bowing. That was really fun. Do Europeans kiss?) They also do this at the Our Father with their neighbors, even though it isn't in the Ritual. Is this bad? Not sure...you could argue that they're adding to the Mass, which not even priests should do, but you could also arguing that they're Christianizing an otherwise secular gesture.
There is a great understanding of the sacredness of space in this culture, so it's natural for them to have LOTS of space between the people and the altar, and for this to be totally cool. (In contrast, some Africans or Hispanic cultures love to go right up to tabernacles and monstrances to touch and pray.) Here, there's a definite "holy of holies" and something untouchable about the Blessed Sacrament. That attitude in their culture (that everyone has their space and you don't trespass) is probably from their history, but it's serving them well at Mass!
Everyone is quiet during the homily. Academic achievement is prized in this culture, and I suppose that's probably helping them. On the other hand, they love partying, so perhaps a third of them are dozing off or distracted, bored. I wonder which one will win out as this little community continues in faith!
Hmm, there are female altar servers and women on the altar. Don't get me wrong, I love women. But I don't think this culture has a huge understanding of priestly celibacy and the otherness of Holy Orders as alter Christus capitis. There hasn't been much interest amongst the young men in vocations to the priesthood, either. Could it be that the female presence on the altar is a sign or symptom of this misunderstanding? I hope the gentle teaching of the Church can help the whole community understand the value of celibacy and the value and uniqueness of the priesthood.
Although there is much singing during the Communion of the faithful, almost everyone is reverent. There is no altar rail in this church and the people mostly receive in the hand, although some receive on the tongue while standing. Almost everyone receives communion. Maybe this is a childlike trust; possibly, some are receiving our Lord unworthily, but who am I to judge? I leave it in the hands of the pastor of this young little flock. There was a great deal of singing (even by the people) after all had received--which is not ideal, since some moments of silent communion are appropriate with the Divine Guest--but this is a child's form of prayer, so that might be the intention and the best thing to do. Some of the people abstained from singing and were silent.
After Mass, there was an enormous hubbub as everyone talked about life, children, schools, activities, and everything else. What a vibrant community! There are flowers at statues of our Lady, the Sacred Heart, St. Joseph, and St. Anthony. I think I'll go back soon.
This might not come as a shock to you, but I am describing my home parish in the post-Christian west. Does your home parish impress you when conceived of as a small and newly-converted community in a deeply pagan culture? In some ways, that is what we are. So two pieces of advice:
- To traditionalists: do not worry. Our culture is now mission territory; don't be shocked that we have primitive churches. Instead, sweetly nurture the poorly catechized and see the good in them to help increase it.
- To those who have no idea what a "traditionalist" is: you might also not know how amazing the Church's history, liturgy, and theology can get (not to mention the art). Strive for maturity in the faith and dig into the patrimony of our Church.
Friday, September 20, 2013
Don't Rock the Boat! Homosexuality and Gender Identity, Medically Speaking
 Caution while challenging the freedom of gender identity! You get called in with three attendings and they have a very polite discussion to make sure you toe the party line.
Caution while challenging the freedom of gender identity! You get called in with three attendings and they have a very polite discussion to make sure you toe the party line.After our lecture on psychosexual disorders during the psychiatry clerkship, the faculty physician asked whether there were any questions. She is a prim older woman, an excellent and compassionate clinician that I had the privilege of shadowing for a week.
I piped up, because she had just talked about gender identity disorder. "I know homosexuality isn't in the DSM-IV," I said, "but I'm confused about the stage a gay or lesbian person is in right before they come out, when they're uncomfortable in the societal role they're in. Isn't that GID? What I mean is, why is GID a disorder and not homosexuality?"
Oops. I didn't mean to finish that way. I wasn't trying to evangelize or start anyone's wheels turning. Seriously. I just wanted to know how this was consistent. (It turns out there is an answer and I understand that this is sort of consistent now. More on that below.)
Well, the prim psychiatrist asked my peers whether they could answer, and they could. After I had been given an answer, the professor said we could take a break until the next lecture. I stood to get a glass of water as my peers also stood to stretch or get a snack. But I was stopped before I got my drink by the lecturer, who said, "why don't we go ask Drs. J and K about your question?" I obliged, and followed her to another room, where two other psychiatry faculty were lunching and talking.
The lecturer and I sat down, completing the four points of a square. "I will share with you," she said to her colleagues, "a question [mmatins] brought up about gender identity disorder." They mused. They gave the same answer my peers had.
Somehow I got the impression I was being given a talking-to. I was suddenly acutely conscious of my conservative dress and crucifix. Perhaps it was the arrangement of the room, or the abruptness and apparent formality of the meeting, or the fact that they gave the same answer my peers had, or the fact that I was alone with three faculty members, all of whom (I am reasonably confident) disagree with me about whether homosexuality is a disorder.
Anyway, nothing happened and everything was pleasant. I and the professor giving the next lecture left the room. Just an interesting experience....
So, FYI, GID is something described in younger patients (i.e. children under twelve) who are uncomfortable with their gender and its non-sexual dimensions such as dress, play, and future societal role. Homosexuality is described in patients who are sexually attracted to members of their sex. They can identify as masculine or feminine, a unique combination of both, a fluid (throughout life) combination of both, or neither but the defining characteristic of homosexuality is sexual attraction to members of the same sex. GID patients are uncomfortable in their bodily gender; homosexual patients are sexually attracted to the same sex.
It's not impossible that a person with GID be later attracted sexually to persons of their same original biological sex, nor is it impossible that a homosexual person have some discomfort with all the accoutrements of their biological sex. But these persons may carry two diagnoses. I still do not understand why "trans" adults cannot be diagnosed with GID. My attending raised this question but I didn't press it.
So, the moral of the story: pray for children with GID whose parents may be tempted to permit the children to undergo sex-change surgery. Pray for "trans" adults with undiagnosed (not-medically-real-according-to-DSM5) GID who are doing the same thing. Pray for LGBQ adults, who are attracted to members of the opposite sex. And be careful as we (prayerfully and charitably) rock the boat.
AS ALWAYS THIS BLOG IS NOT TO REPLACE THE CARE AND DIAGNOSIS OF TRAINED PROFESSIONALS.
Wednesday, September 18, 2013
A day in the life of Family Medicine
Whew! Family Medicine is over and I am now 12 weeks into third year. I am so tired! This post is not unified or well written; it's a journal entry and nothing more. My advise: skim or skip.
Most of the mornings started at 8:00am in Family Med. I would go to 6:30 am Mass and then drive to a suburban hospital where there was a family practice group and a family practice residency program. I spent two weeks in the group and two weeks with the residents. A week of lectures and one week with the residents on their inpatient medicine service rounded out the clerkship.
I would eat breakfast in my car, parked in the church parking lot. Sometimes, I would see my mom as she arrived for work at 7:30 (she works at the primary school associated with our parish). I arrived at work at 7:45 and started clinic at 8:00.
 I liked working in the residency clinic more than the group practice because it was more education-driven. I was also more like my preceptors: in the group, I worked with a doc who'd been practicing for ten years before I was born. He was so experienced (and maybe a little sloppy) that he hardly collected any history before announcing a diagnosis. He also typed with two fingers, and so was really slow with the EHR. I pitied him--even though I had about twenty minutes of training, I picked up at least as much as he had in the few weeks I was with him!
I liked working in the residency clinic more than the group practice because it was more education-driven. I was also more like my preceptors: in the group, I worked with a doc who'd been practicing for ten years before I was born. He was so experienced (and maybe a little sloppy) that he hardly collected any history before announcing a diagnosis. He also typed with two fingers, and so was really slow with the EHR. I pitied him--even though I had about twenty minutes of training, I picked up at least as much as he had in the few weeks I was with him!
I was closer to the residents' age and experience level and, although I always treated them with the respect their degree and position commanded, I felt more comfortable imagining myself in their shoes. "Family medicine wouldn't be so bad," I thought, when I worked with them. (When I worked with the older doc, I thought, "this definitely isn't for me.... Advising all these old people to take mustard when they have a cramp even if they have stage III CKD and typing notes until 12:00am...no thanks.")
Morning clinic would wrap up around 12:30 or 1:00, and clinic would resume at 1:30 or 2:00.
During the day I would see between five and ten patients: I would read their chart a little before tapping on the door and introducing myself. I'd ask them what they came in for and question them about their health or problems, and then I'd decide how to examine them and perform the exam. I documented my findings in the EHR and excused myself to "present" the person to my preceptor.
"Mr. So-and-so is a such-and-such-year-old white male with a history of hypertension and diabetes who comes in today complaining of a four-day history of tingling in his feet," I might say. I would describe the pain (or the cough, or the relevant details of his chronic disease) and then the pertinent positives and negatives, before describing my physical exam. "His heart has regular rate and rhythym without murmurs, gallops, or rubs, and his lungs are clear to auscultation bilaterally." Then I was supposed to say my assessment and plan, but frequently I didn't have to do this.
(Parenthetically, it's funny to write all that out, because all that text would become "Pt is a XXyo WM with 4d h/o tingling in bilateral feet....Heart: RRR s MGR, Lungs: CTAB" in the EHR)
The preceptor would ask me questions to which I usually didn't know the answers ("Does he have a family history of heart disease?" "What do you make of his elevated LFTs?"), and we would go see the patient again together. I liked seeing patients myself, making plans for them, and educating them. I really disliked presentations and not knowing enough.
I usually stayed past 5:00pm and got home tired and hungry. My family eats when my dad comes home, which is variable...so that caused some friction until mom told me I should just eat when I get home so that I can go and study. I would get to bed at 10:00 or shortly thereafter following night prayer. Usually, no recreation unless I stole some time to talk with my family, ride bikes, blog, or read.
I enjoyed working the inpatient week because I again got to see patients myself, examine them, and write notes in their charts with my own baby assessment and plan. However, this week I wasn't able to attend Mass, and so I asked our parish priest to give me the Blessed Sacrament before Mass began so that I could go to work early for shift change and rounding.
I was constantly readjusting and struggling to fit in all the things I thought I needed to do: morning and evening prayer, midday prayer, meditation, Mass, formation, work, and family took so much time that studying was almost eclipsed! I saw the result on my NBME, sadly. I would study on Saturdays and on occasionaly weeknights, but it never seemed to be enough. I always felt behind! Family Med contains so many subjects (acute and chronic diseases of every organ system in all ages and both genders! Mwaha!) that I was only confident in about a dozen by the end of the clerkship.
Where is God's will for this time in my life? I feel like I'm working two full-time lives: a medical student who needs to work and study, and a consecrated virgin in formation, who needs to study (different things!) and pray. And both are suffering because of the other! I work but I am tired because I don't get enough sleep and exercise; I study, but only a little bit, so that my work suffers; I study the Catechism (but am ten days behind) and listen to my Faith Foundations lectures (but they go in one ear and out the other b/c I listen to them in the car) and go to formation (where I am so tired they have been letting me go early); and I pray, but am so distracted and tired that I don't perceive God's presence. What needs to change???
My expectations, perhaps? Please pray for me, so that I can see God's will. I finally have a spiritual director here, and hopefully we will meet soon to talk about all this.
On to pediatrics!
Most of the mornings started at 8:00am in Family Med. I would go to 6:30 am Mass and then drive to a suburban hospital where there was a family practice group and a family practice residency program. I spent two weeks in the group and two weeks with the residents. A week of lectures and one week with the residents on their inpatient medicine service rounded out the clerkship.
I would eat breakfast in my car, parked in the church parking lot. Sometimes, I would see my mom as she arrived for work at 7:30 (she works at the primary school associated with our parish). I arrived at work at 7:45 and started clinic at 8:00.
 I liked working in the residency clinic more than the group practice because it was more education-driven. I was also more like my preceptors: in the group, I worked with a doc who'd been practicing for ten years before I was born. He was so experienced (and maybe a little sloppy) that he hardly collected any history before announcing a diagnosis. He also typed with two fingers, and so was really slow with the EHR. I pitied him--even though I had about twenty minutes of training, I picked up at least as much as he had in the few weeks I was with him!
I liked working in the residency clinic more than the group practice because it was more education-driven. I was also more like my preceptors: in the group, I worked with a doc who'd been practicing for ten years before I was born. He was so experienced (and maybe a little sloppy) that he hardly collected any history before announcing a diagnosis. He also typed with two fingers, and so was really slow with the EHR. I pitied him--even though I had about twenty minutes of training, I picked up at least as much as he had in the few weeks I was with him!I was closer to the residents' age and experience level and, although I always treated them with the respect their degree and position commanded, I felt more comfortable imagining myself in their shoes. "Family medicine wouldn't be so bad," I thought, when I worked with them. (When I worked with the older doc, I thought, "this definitely isn't for me.... Advising all these old people to take mustard when they have a cramp even if they have stage III CKD and typing notes until 12:00am...no thanks.")
Morning clinic would wrap up around 12:30 or 1:00, and clinic would resume at 1:30 or 2:00.
During the day I would see between five and ten patients: I would read their chart a little before tapping on the door and introducing myself. I'd ask them what they came in for and question them about their health or problems, and then I'd decide how to examine them and perform the exam. I documented my findings in the EHR and excused myself to "present" the person to my preceptor.
"Mr. So-and-so is a such-and-such-year-old white male with a history of hypertension and diabetes who comes in today complaining of a four-day history of tingling in his feet," I might say. I would describe the pain (or the cough, or the relevant details of his chronic disease) and then the pertinent positives and negatives, before describing my physical exam. "His heart has regular rate and rhythym without murmurs, gallops, or rubs, and his lungs are clear to auscultation bilaterally." Then I was supposed to say my assessment and plan, but frequently I didn't have to do this.
(Parenthetically, it's funny to write all that out, because all that text would become "Pt is a XXyo WM with 4d h/o tingling in bilateral feet....Heart: RRR s MGR, Lungs: CTAB" in the EHR)
The preceptor would ask me questions to which I usually didn't know the answers ("Does he have a family history of heart disease?" "What do you make of his elevated LFTs?"), and we would go see the patient again together. I liked seeing patients myself, making plans for them, and educating them. I really disliked presentations and not knowing enough.
I usually stayed past 5:00pm and got home tired and hungry. My family eats when my dad comes home, which is variable...so that caused some friction until mom told me I should just eat when I get home so that I can go and study. I would get to bed at 10:00 or shortly thereafter following night prayer. Usually, no recreation unless I stole some time to talk with my family, ride bikes, blog, or read.
I enjoyed working the inpatient week because I again got to see patients myself, examine them, and write notes in their charts with my own baby assessment and plan. However, this week I wasn't able to attend Mass, and so I asked our parish priest to give me the Blessed Sacrament before Mass began so that I could go to work early for shift change and rounding.
I was constantly readjusting and struggling to fit in all the things I thought I needed to do: morning and evening prayer, midday prayer, meditation, Mass, formation, work, and family took so much time that studying was almost eclipsed! I saw the result on my NBME, sadly. I would study on Saturdays and on occasionaly weeknights, but it never seemed to be enough. I always felt behind! Family Med contains so many subjects (acute and chronic diseases of every organ system in all ages and both genders! Mwaha!) that I was only confident in about a dozen by the end of the clerkship.
Where is God's will for this time in my life? I feel like I'm working two full-time lives: a medical student who needs to work and study, and a consecrated virgin in formation, who needs to study (different things!) and pray. And both are suffering because of the other! I work but I am tired because I don't get enough sleep and exercise; I study, but only a little bit, so that my work suffers; I study the Catechism (but am ten days behind) and listen to my Faith Foundations lectures (but they go in one ear and out the other b/c I listen to them in the car) and go to formation (where I am so tired they have been letting me go early); and I pray, but am so distracted and tired that I don't perceive God's presence. What needs to change???
My expectations, perhaps? Please pray for me, so that I can see God's will. I finally have a spiritual director here, and hopefully we will meet soon to talk about all this.
On to pediatrics!
Friday, September 13, 2013
My Brush with Euthanasia: Forget Not Love
 Euthanasia is a terrible thing. I had a brush with it about a month ago while on a geriatric ward. This might surprise and scare you. Just to clarify, this actually happened. I am exaggerating nothing.
Euthanasia is a terrible thing. I had a brush with it about a month ago while on a geriatric ward. This might surprise and scare you. Just to clarify, this actually happened. I am exaggerating nothing.I was reviewing an older patient's chart at the nursing station before rounds. This person was on dozens of medications. The home medication list was three pages long. Everything was carefully listed by doses, times, and routes (oral, otic, ophthalmic, topical, nasal...), but the sheer volume was overwhelming. On top of the drugs for medical and mental problems, there were various prescriptions and OTC remedies to cover side effects of the first drugs.
(If polypharmacy is new to you, then let me explain how these lists grow. A man of 64 on no medicines has some chest pain and goes to his doctor. He leaves with instructions to take a baby aspirin every day. And, because his blood pressure was high, he also leaves with a prescription for a water pill and a blood pressure medicine.
(Fast forward four years. Despite his daily three drugs, the man ends up in the hospital with a heart attack. He leaves with a stent, an antiplatelet agent, a pill for cholesterol, and an ACE inhibitor.
(Fast forward another eight years. Our man seems to be getting lost around the house and can't balance the checkbook very well any more. He's put on two drugs for dementia. Thyroid replacement is added because a thyroid test was high. His wife added a multivitamin, CoQ10, and glucosamine to keep him healthy after that fall he had last Christmas, and he also has nitroglycerin on hand, for that chest pain that started all this. He's now up to a dozen drugs, not counting any OTC painkillers, eye drops, or occasional antibiotics.)
Back to my story: I looked at the three page list of medicines in my hand, aghast. How burdensome this regimen had become for the patient and caretakers! What was this person's quality of life like, with so much intervention? This all seemed like artifice to replace the functions of a failing body. It seemed like torture to prolong a life. And for what?
I looked up from the page out to the patients beyond the nursing station counter. Half of the patients on this ward seemed over-medicated to me. They sat in their wheelchairs unaware of their surroundings. Other professionals I had learned from, including very compassionate hospice nurses, liberally took patients off medicines toward the end of life. I liked this palliative, simplifying approach. Too much medicine is a cloying thing, a clinging to numbers or days. I thought to myself, "why not just take this patient off everything and let her go peacefully?" No more surprise bruises from aspirin, no more dizziness from the blood pressure pills. No more bother with all these pills and suppositories and drops.
But today I looked at her three page list, I saw one problem with the remove-the-medicines approach. Two of this patient's medications were high-potency antipsychotics in high doses. And the rest of the regimen was like a teetering game of Jenga: remove one thing, no matter how extraneous, and the rest collapses. I groaned inwardly. We could not let this person off her medicines...it would not be peaceful or safe, and it would not improve her quality of life. If medication withdrawal couldn't be done, what could? How could this patient and her caregivers be relieved of all this?
"What if," I thought, "What if we just gave a little too much of something?"
Immediately I was alarmed. Where did that thought come from? Did I just suggest to myself that I should euthanize a person? I had. I was thinking about giving something (e.g. a benzodiazepine) to let her just slip away. I was horrified at the thought I had just produced.
How did I get to that point? I was thinking about burdens and quality of life! How did I go so far astray?
Looking back, I realized that in the few days I'd worked on that ward, I had taken on the attitude of the attendants there. They shouted at the patients from their chairs in the nurse's station and loudly talked and laughed about them like children or animals. Giving medications in such big and complex regimens was a chore. They didn't love. And although I detested this and really couldn't wait to be off that ward, it rubbed off on me! Writing so many orders--what a chore! Working on this ward--what a burden! So, as I was looking at that medication list, I was not loving the person, even though I was pitying them.
And as soon as I forgot about love, I forgot about the meaning of life, the dignity of persons, the mystery of each soul's holy journey, and the importance of suffering in salvation. Who knows whether that person on three pages of medication was becoming a great saint or mystic? Beneath the shroud of dementia and crippled limbs, under the veil of an incontinent, flailing old woman, perhaps God was adorning an exquisite saint. Perhaps in heaven her beauty and nobility will be breathtaking. And moreover, what if her suffering was saving my soul? Yours? Our country, our world? How could I dare to know? (Job 38 comes to mind.) Certainly, simplifying her regimen with palliation in mind isn't a bad idea, but I only safely stay in that mindset when I remember love.
So forget not love. It's a deadly mistake.
Sunday, September 8, 2013
My Plans for the Future
I want to be a doctor to the whole person and that includes maintaining education in primary care areas as well as in OB and gynecology. I also think having an in-house NFP teacher, in-house dietician, and in-house psychologist (IPS, anyone?) would be excellent. A multispecialty group practice appeals to me, so that whatever practice I have can be a patient-centered medical home.
Of course, part of the future is offering women's healthcare in accord with Catholic teaching, which is to say to offer the best women's healthcare. Perhaps I would imitate Mystical Rose or Caritas Complete Women's Care or the Vitae Clinic with my own private practice. Maybe I would imitate Tepeyac Family Center/Divine Mercy Care and become an ACO.
 |
| St. Guiseppe Moscati, doctor to the poor (well, the very romanticized movie version) |
Becoming a subspecialist in a maternal-fetal-medicine (MFM) also appeals to me. As an MFM, I could operates on the unborn, work with infertile couples, and take care of very high-risk pregnancies, also appeals to me. I have this dream of showing people how human the unborn are, how like us and how worthy of attention they are. What if we could re-implant babies who implanted in the wrong place? What if we could treat things like Potter's syndrome? (What if we could pull out all the "medical reasons" for abortion?) There are other advantages to this idea, too: my refusal to prescribe contraceptives and refer for abortions might irk fewer colleages if I was in MFM and had fewer occasions to do these things.
 |
| ♪ MFM ♪ |
If I started a women's healthcare center and used midlevel professionals (NPs and PAs) and allied health (nurses, MAs, psychologists, social work, and dieticians) to establish a large group of primary care and OB/GYN providers for women, we could serve the poor and offer cutting-edge infertility and prenatal service with excellent gynecology. That's the future I'm working for now. (Now, if you'll excuse me, I need to go study for a shelf exam so that people don't laugh in my face when I say I want to do a surgical subspecialty.)
Monday, September 2, 2013
Fatigue!
In the past five or six weeks I was dragging. It was hard to stay focused, hard to love others, and hard to do all my duties with attention and comfort. I felt sleepy during the day and everything took more energy. I was thinking, "I'm just in desolation," or "I don't really have what it takes to love others," and "maybe I can't be a physician...I just don't have it in me...." Finally, when two wise people (my biological and spiritual mothers) independently told me to go a doctor, I did. I was in sleep debt and had a microcytic (probably iron-deficient) anemia and had lost eight pounds. I really dropped the ball on taking care of myself!
Have you read Jen Fulwiler's post about struggling against circumstances? She says everything I want to say about this, and much more (about motherhood, etc).
I'm doing much better now, partially due to the relief that some of my sluggishness was physical (nobody's forgotten that a bunch of it is still spiritual...I still have a hard time loving people even when I'm brimming with energy and consolation). And now I'm getting more sleep and food and iron. Thanks be to God for bodily helps to holiness!
Sunday, August 25, 2013
Vocation story
 I have recently finished writing my vocation story! I was hard and easy at the same time. I felt like I should get it "right," and somehow have the perfect version...but that just resulted in me never typing anything. Finally, one day I just sat down and told it. Deo gratias.
I have recently finished writing my vocation story! I was hard and easy at the same time. I felt like I should get it "right," and somehow have the perfect version...but that just resulted in me never typing anything. Finally, one day I just sat down and told it. Deo gratias.
Thursday, August 22, 2013
Ultrasounds before Abortions
Have you ever been so angry you couldn't speak? I have been meaning to write about a talk I attended, given by Dr. Rebecca Kukla on ultrasound viewing before abortion. Dr. Kukla argued that ultrasound screening has become a ritual in our society to establish parenthood and add (prematurely and irrationally) a new member to the family. Performing an ultrasound and explaining the findings to a woman desiring to end her pregnancy would thus cause unnecessary and severe psychological trauma. She also argued that this imposed moral harm on physicians as it required them to violate their fundamental duties to patients.
I have been meaning to write this post since January. I have kept the folded-up flier from the talk in my desk since then. There it sat, outlasting the semester, my STEP studying, and my move to a different city. Usually, when I keep a piece of paper as a reminder to complete a task (e.g. a blog post, or mailing something, or running an errand), the having of the paper bothers me just enough to make me want to complete the task. But this time, I preferred to keep the paper rather than write the post. I just couldn't do it.
Every time I sat down to do it I would formulate the ghost of an argument, take out the paper, unfold it, look at it, and recall the tone and content of the argument. The first few wisps of a post that I had would evaporate as I would become angry. Not desiring to be angry, I would just put the paper and the idea away.
Today I realized the pattern. And now the flier is in the trash, but I have a decision to make (I am literally making this decision as I type). I can either write the rebuttal now, or I can just forget about it.
I am still too angry for a level-headed, reasoned argument, so if you read this, Dr. Kukla, please excuse me as still young and full of idealism. I will strive to be professional, though.
Before most minor surgical procedures that require general anesthesia (e.g. cholecystectomy or gall bladder removal), an ultrasound or other imaging is done. Vaginal ultrasound is quite common in gynecology. It also doesn't stand out as uniquely invasive. (Ultrasound for cholecystectomy gets to the bile duct via the mouth, and I'm sure you can imagine how they stage colon cancer). Abortions actually become more like the minor surgical procedures they're touted to be when an ultrasound is performed. I would hope they're done anyway.
Adequate bedside manner during any exam or procedure in which a person is awake but unable to interpret the findings includes explaining the findings. "Mrs. Anderson, your lungs sound normal." "Ms. Patel, the skin biopsy is almost over and your back looks good." "Mr. Deere, this darkish color on the ultrasound means you have a lot of fat in your liver." Let's encourage abortionists to have good beside manner by requiring them to describe the findings. I would hope most of them do anyway.
Dr. Kukla's concludes that ultrasounds like this impinge on the physician's duty to do no harm, but she happily supports the procedure that follows, which will leave 14% of the women who undergo it with full PTSD (slide 42). (For reference, 15.2% of Vietnam vets have full PTSD.) Abortion increases the risk of suicide to 650% (slide 74), substance abuse (61 and following), and depression (9 and following) is considered desirable, so desirable that even medically legitimate restrictions are deemed morally intolerable.
I think that's all I have to say. Dr. Kukla and I agree that vaginal ultrasound cannot be considered a kind of "rape," and we also agree that it's not ideal that these regulations come through a governing body (we'd both prefer they come through professional organizations). But I find her basic attitude (defending abortion while objecting to an ultrasound) to be inconsistent.
I have been meaning to write this post since January. I have kept the folded-up flier from the talk in my desk since then. There it sat, outlasting the semester, my STEP studying, and my move to a different city. Usually, when I keep a piece of paper as a reminder to complete a task (e.g. a blog post, or mailing something, or running an errand), the having of the paper bothers me just enough to make me want to complete the task. But this time, I preferred to keep the paper rather than write the post. I just couldn't do it.
Every time I sat down to do it I would formulate the ghost of an argument, take out the paper, unfold it, look at it, and recall the tone and content of the argument. The first few wisps of a post that I had would evaporate as I would become angry. Not desiring to be angry, I would just put the paper and the idea away.
Today I realized the pattern. And now the flier is in the trash, but I have a decision to make (I am literally making this decision as I type). I can either write the rebuttal now, or I can just forget about it.
I am still too angry for a level-headed, reasoned argument, so if you read this, Dr. Kukla, please excuse me as still young and full of idealism. I will strive to be professional, though.
Before most minor surgical procedures that require general anesthesia (e.g. cholecystectomy or gall bladder removal), an ultrasound or other imaging is done. Vaginal ultrasound is quite common in gynecology. It also doesn't stand out as uniquely invasive. (Ultrasound for cholecystectomy gets to the bile duct via the mouth, and I'm sure you can imagine how they stage colon cancer). Abortions actually become more like the minor surgical procedures they're touted to be when an ultrasound is performed. I would hope they're done anyway.
Adequate bedside manner during any exam or procedure in which a person is awake but unable to interpret the findings includes explaining the findings. "Mrs. Anderson, your lungs sound normal." "Ms. Patel, the skin biopsy is almost over and your back looks good." "Mr. Deere, this darkish color on the ultrasound means you have a lot of fat in your liver." Let's encourage abortionists to have good beside manner by requiring them to describe the findings. I would hope most of them do anyway.
Dr. Kukla's concludes that ultrasounds like this impinge on the physician's duty to do no harm, but she happily supports the procedure that follows, which will leave 14% of the women who undergo it with full PTSD (slide 42). (For reference, 15.2% of Vietnam vets have full PTSD.) Abortion increases the risk of suicide to 650% (slide 74), substance abuse (61 and following), and depression (9 and following) is considered desirable, so desirable that even medically legitimate restrictions are deemed morally intolerable.
I think that's all I have to say. Dr. Kukla and I agree that vaginal ultrasound cannot be considered a kind of "rape," and we also agree that it's not ideal that these regulations come through a governing body (we'd both prefer they come through professional organizations). But I find her basic attitude (defending abortion while objecting to an ultrasound) to be inconsistent.
Tuesday, August 20, 2013
Oh dear. Family Medicine.
So, on the first day of the family medicine rotation, the clerkship director gave a presentation about family medicine--what it is, why one would go into it, etc. And something seriously bizarre happened.
I have wanted to become an OB/GYN for something like eight years. Family med has always been the second choice, but it was always dismissed because of things like a preponderance of metabolic syndrome (ugh), no surgical components (double ugh) and excessive government oversight (triple ugh).
But as that clerkship director was talking, I began to seriously think family med deserved a more than serious look. I began to really want to be a family doctor. I began to think so seriously that I started making a list of pro's and con's on my orientation packet. And I didn't even call the con's "con's," I just wrote them under a list I labeled "Hm."
Hm
I have wanted to become an OB/GYN for something like eight years. Family med has always been the second choice, but it was always dismissed because of things like a preponderance of metabolic syndrome (ugh), no surgical components (double ugh) and excessive government oversight (triple ugh).
But as that clerkship director was talking, I began to seriously think family med deserved a more than serious look. I began to really want to be a family doctor. I began to think so seriously that I started making a list of pro's and con's on my orientation packet. And I didn't even call the con's "con's," I just wrote them under a list I labeled "Hm."
Hm
- I would miss the OR and surgery. I really like anything that requires manual dexterity.
- Every time someone suggests FM as a way to go, they mention rural care and mentally I go "ACK! NO!!" I don't want to do rural care. Sorry, but I want to stay in my city! I'm happy to serve the urban poor, and that's what I want to do, but no rural care until my parents are deceased. That's the law (right now).
- The government looooooooves primary care. FM is the answer to ALL Obama's problems. Hence, I don't want to go into a field where I become Big Brother's employee or marionette.
- SYNDROME X. Nuff said?
- I love to educate, and that is what a lot of FM is. I love to bring people up to speed by going to meet them where they are and encouraging them. That was in my personal statement.
- Better hours than OB/GYN!
- FM is actually the answer to MANY of the nation's healthcare spending problems. I don't want to be a governmental employee, but it would be good to actually help with a big problem.
- I used to want to be a family doctor but somewhere along the line I learned that the golden age was over and family docs were referral machines (it was a job for the dumbest med students). But I don't think that's true anymore, not after meeting some of the faculty here and elsewhere.
- I was complaining after psychiatry that I wish I'd become a therapist instead of an MD, since they seemed to do more for people. FM would be more like the therapist and less like the drug pusher.
- It's natural. It's basic. I like that.
- It's the most helpful, in terms of morbidity and mortality.
- I LOVE the idea that one person has one doctor, or at least one main doctor managing the team. The patient centered medical home model really appeals to me, as does the ACO, multispecialty practice, and group visit.
- I like the idea of managing complexity. Although I don't want to manage everyone's unmanageable syndrome X, I do like to use my brain. (IMED, is that you calling?)
- I like the idea of being able to everything (ish) for the poor.
- It has a lower income.
- It's almost all outpatient. One thing I didn't like about psych and a few of the docs I've shadowed is that they have inpatient and outpatient, and spend a lot of time driving.
- It has a shorter residency AND (get this) you can do a year-long fellowship in OB and then *poof* I would have spent the same amount of time (four years) getting ready for prenatal care as I would in an OB/GYN residency. I'd miss the surgery (except C-sections) but I would be out from under the thumb of ACOG and not responsible for IUDs, sterilizations, and IVF while still managing what matters most to me anyway (prenatal care, birth, miscarriage, prenatal hospice, NFP, STDs, sex and abstinence ed, and postabortion recovery).
- I might be able to do residency more easily in my home city. And that means, I might be rotating where I will eventually be a resident. (Better shape up!)
Subscribe to:
Posts (Atom)







.jpg)


