I will now discuss the stuff of third year that is not happy
and glamorous. Having a blog places slight pressure on a person not to whine.
But not to disclose the negative parts of medical school would be dishonest. So
it’s time to air a few grievances, and (because I can’t seem to
not do
this) discuss morality and holiness at the same time.
At some point during my third year, I got very demoralized.
It’s hard for a person who wants to do great things well (and is used to doing
great things well) to find herself unable to hope even for mediocrity.
One response to this predicament: Ah, what a chance to grow
in humility!
 |
| THIS IS AWESOME. |
"Ah," goes this response, "I have had many peers, past and present, who have struggled to get the things I’ve gotten, like A’s and letters of recommendation and leadership positions and success…. Now, God is making me more like them, to help me see that they are my brothers in everything. I have nothing of my own and am happy to have God, because I truly lack nothing."
Another and much more human response to this predicament:
 |
| THIS IS TERRIBLE. |
In its severest form, this disappointment becomes sadness, loneliness, isolation, depression, and despair.
It was a war between these two responses for the second half
of third year. However, it is old news that 1) I am a little soul and 2) there's a war going on in me between holiness and not-holiness. God is exerting Himself to the maximum and
employing all kinds of things (sacraments, virtues, habits, circumstances,
living people, dead people, people I’ve never laid eyes on, angels, and even
me) to make me like Himself. On the other side are all kinds of things
(occasions, vices, habits, circumstances, living people, dead people, people
I’ve never laid eyes on, angels, and especially me) persuading me to stay in my
nice little hidey-self-in-hell-hole.
But morality aside for a teensy moment: seriously! This year
was so demoralizing at times!
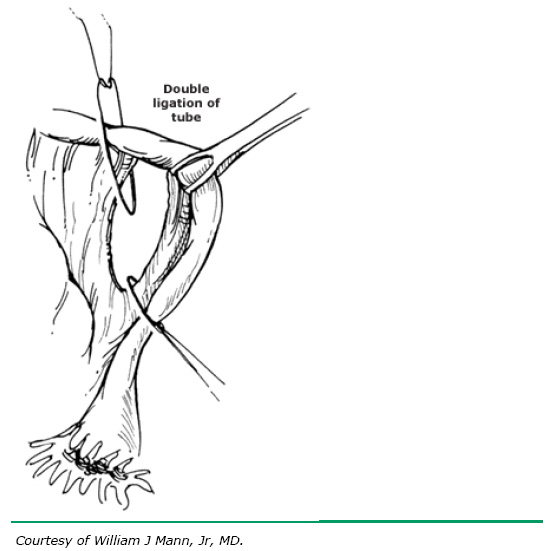
Do you have any idea what it is like to stand in a surgery,
not allowed to do anything except trim suture? Somebody ties a knot around
[whatever], and I come in with scissors and snip it. That is 90% of my
intraoperative action. This is especially painful because I’ve been given great
responsibility and responded rather well to in the past. I wish I could speak
my mind in those ORs.
“You know, I am a person.”
Snip.
“With an intellect.”
Snip.
“A rather
good intellect.”
Snip.
“And I have pretty good hands, too. Did you know I paint?
And I’m handy around the house.”
Snip.
“And if you let me stick-tie the ovarian vessels/close the
fascia/dissect adhesions/use a bovie/debride dead tissue/MANY OTHER EXAMPLES, I
bet I could do it.”
Snip.

The worst part is, I am not even permitted to stupidly cut
as I like. I am chided because I am not doing it properly. Since the clinical
years of medical school are a dizzying merry-go-round through services and surgeons,
I can never acquire expertise in one thing. Many have pretened to, but no one
ever has, given me a comprehensive lesson in how to properly cut all types of
suture in all places according to the preferences of all surgeons. (I expect
even the Eternal Father would have difficulty with this one. Just kidding,
Abba.)
“Whoa!” says one surgeon. “Too short.”
Or again, the surgeon is uncomfortably silent after I cut. I
timidly ask, “too long?”
At least I have never cut someone’s knot. There was once
when I took the blame for a broken knot. A few minutes after I snipped, one of
the resident’s knots came undone. To save the resident face, I said, “Oh, I cut
your knot, didn’t I. I’m sorry.”
I became the queen of taking flak this year. There was an
“Oh, thank you,” after every correction; there was a sincere-sounding “I’m
sorry,” after every action someone objected to.
Today, while snipping, I grew less and less successful. I
began to wonder whether there was a problem with the scissors. Surgeons and
residents are quick to ask for a different instrument if the one they’re
holding does something silly or inefficient. Not being a surgeon or a resident,
I waited out my silly, inefficient instrument for a good five more snips. While
I waited, a new scrub tech clocked in. This meant I lost the rapport I’d built
up with the first one (my pulling a gown and gloves, helping in setup, etc) I
didn’t think anything of this at the time, but now I wonder whether er shift
change made a difference in the answer I received when I eventually asked, “Do
you have another pair of scissors?”
There are at least four pairs of scissors in almost every
set. I know because I know their names: curved Mayos, Mets, tenotomies. There
are also Potts and Dietrichs, but even I wouldn’t use those for suture (now I’m
just showing off how many types of scissors I can name without looking things
up). The suture scissors are called “heavy sciz” by some, but their real name
is straight Mayos. Technically, you’re supposed to use the straight Mayos for
stuff,
like foam, suture, and mesh. Cutting these undelicate things with the better
scissors would dull the blades and damage tissue. But I’ve seen surgeons get
frustrated with a pair of straight Mayos. They drop them to purposefully
exclude them from use, then start to use the curved Mayo’s or the Mets. I’ve
even seen someone use the tenotomies. So
certainly it would not have
been absurd for me to use a different pair of scissors. But what did the scrub
tech say?
“Is it the scissors, or is it
you?”
I felt like exploding.
“
Please,” I wanted to say, “even if it is me, could
you think of a different way to say it? Maybe ‘show me how you’re cutting’? Or
maybe, just
maybe you could humor me? I humor people to ridiculous
extent. Could you just hand me the curved Mayos? Maybe then I’ll learn that it
is, in fact, not the scissors. And you know what else? Even if it’s not the
scissors, I don’t like that you said ‘me,’ as if I/me/my
person is a
problem. My technique might be lousy, but why the ad hominem? Why do
I become
a problem because I don’t cut suture properly? And anyway, who has taught me how
to cut? No one! I have had to cobble things together myself!”
 |
See the med student, doing nothing?
Oh wait, I forgot to get them in the camera view. |
But I said, smiling doormat that I have become, “Oh, probably me.” And
she said what I should have been doing. My success was unchanged: some good
cuts, some lousy ones. In retrospect I think the scissors were fine and I was
fine. The problem was that the incision was getting deep (down to the
retroperitoneum) and therefore the sutures were getting further and further
away from me. When you have to stand on tiptoe and crane your neck and reach to
cut something, nothing works quite as well. I can’t wait to be the surgeon or
the resident and have a legitimate place to stand so that I can see the
operative field all the time.





















 (That may or may not be where I'm living; I didn't even check before I used the picture; thanks to Kim Briggs)
(That may or may not be where I'm living; I didn't even check before I used the picture; thanks to Kim Briggs)










