"Yes, it could," he answered. He beat around the bush, though, so I asked him point-blank: "Is blocking implantation abortifacient?"
Here's his answer. The two ellipses are his own, almost as if he's hemming and hawing in discomfort:
That's an ethical discussion, [mmatins]. I think most patients who are concerned and ask about it think of it in that regard...to me, it's not quite the same as intentionally ending an existing pregnancy, but it gets at the argument of when life begins: is it at conception, at implantation, at birth, etc...How can someone say "that's an ethical discussion" and mean "that's a discussion I can't have?" Ethics permeates everything we do; it is the science or art of acting well! Ethics is so important to reproductive medicine, and it is precisely there that it is treated like it is irrelevant or relative.
When Obama tried this move I thought "psh, come on." When an OB/GYN tries it, I moan and think "who gave you a license??"
And imprecision we wouldn't put up with elsewhere: "it's not quite the same." Not quite? So how much? Should we put up limits? Should we establish best practice guidelines? Should we pass a law? Should we at least tell patients it's "not quite them same" instead of telling them "no, Mirena doesn't cause abortions"?
The insanity continues, though. I emailed a second professor. This woman is a brilliant maternal-fetal medicine OB/GYN with whom our whole class is in love over her funny (and manageable!) lectures. Here is what I asked her:
In your work you monitor, treat, and even operate on babies during delivery or even longer before they're born. I'm trying to reconcile this concern we have for fetuses with medical and surgical abortions. Sometimes we make sure babies are okay; other times we make sure they regress or are removed. How is this consistent?She replied:
That is a big question and [there are] so many debatable topics possible there. I think a lot of the answer, from my standpoint, goes into counseling patients about what we know about certain diseases and therapies for intrauterine treatments. There will be many more in the future I'm sure, so right now, sometimes we are limited in fetal therapies. As for elective terminations, the same applies for extensive counseling for the patient. risks and benefits for terminations as well as for fetal procedures are key for patients making these decisions. Not sure if that answers your question. MFM is a very challenging field as there is very seldom a distinct line that helps us decide what therapies work....and very rarely, if ever, is there a predictive fetal test that is 100%! This makes the job of an MFM always challenging, and I am sure the role of the pregnant patient very frustrating and complex.The advice to counsel patients completely is good (I will always do that) and the words about difficulties should be appreciated as coming from one with experience. But finally, she didn't answer my question. I replied, clarifying my question to
..."is the fetus a patient?" The answer is "no" in elective termination but "yes" in laser ablation for poly/olis (for instance). Why does the answer change?And she said simply:
So, it seems that in the OB world, in regards to procedures, many decisions are made regarding the viability of the fetus (ie: would it be able to survive outside the uterus) at the time of the procedure.I asked her whether elective terminations will be threatened by advances in NICU, and haven't heard back yet. But the answer to the question "how do pro-choice doctors think?" seems to be...they don't. When I ask them a question, they skirt it, and refer to vague principles about patient counseling and changing technologies that don't hold water.
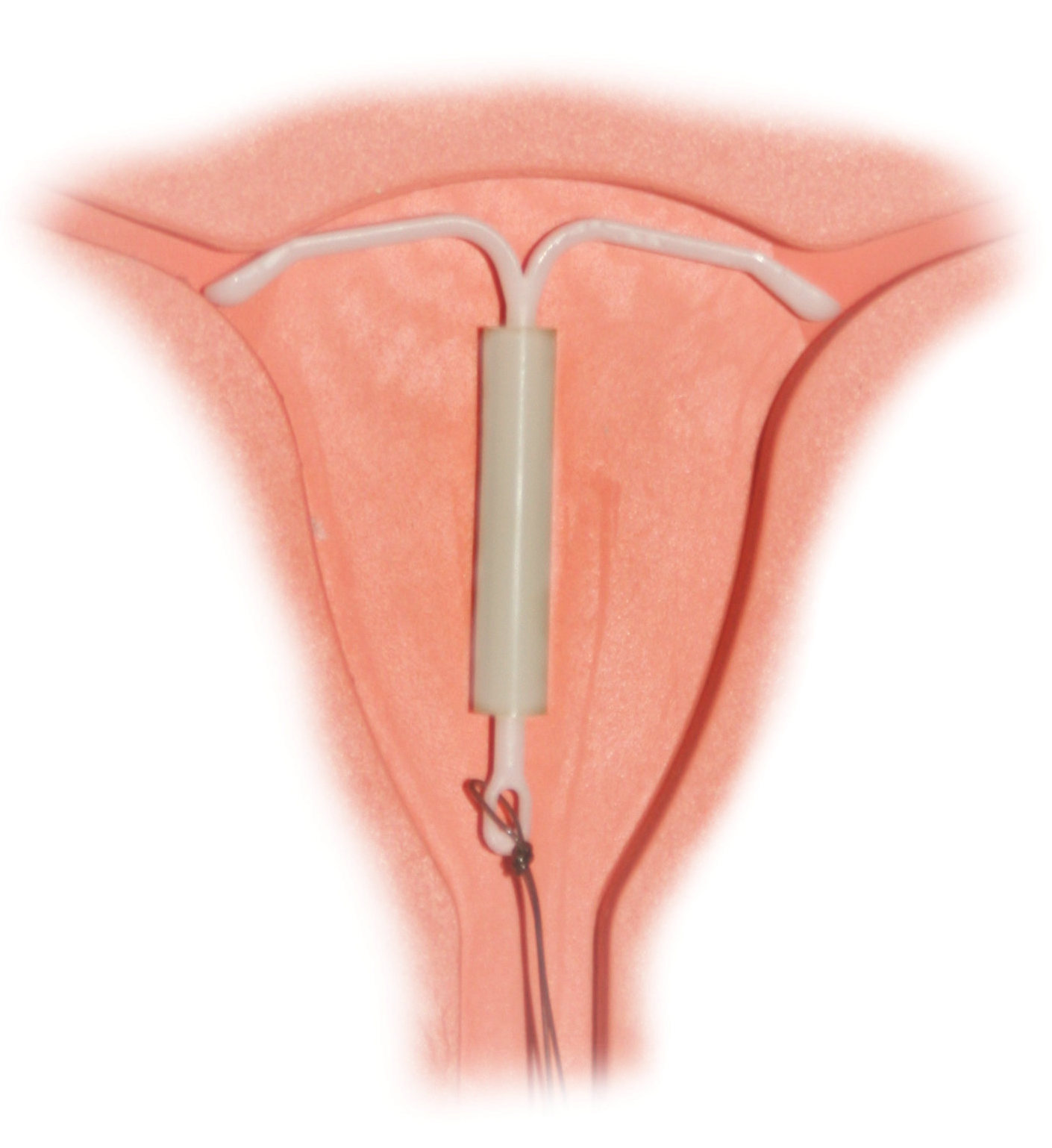
I don't read intentions onto this omission (rather, I will hold that they are doing their best with what they have been given and I pray that they live long and never resist grace). At the same time, they just don't put two and two together. Stay tuned. We had the contraceptives lecture today, so this blog will scale the cliffs of insanity again before May.







.jpg)

